 With the first performance year of the Merit-based Incentive Payment System (MIPS) drawing to a close, you may have just started getting accustomed to how MIPS reporting works. Although the 2018 MACRA final rule introduced changes to how MIPS performance data should be captured for the upcoming performance year, it may be a relief to hear that largely the changes just build upon the existing 2017 regulations.
With the first performance year of the Merit-based Incentive Payment System (MIPS) drawing to a close, you may have just started getting accustomed to how MIPS reporting works. Although the 2018 MACRA final rule introduced changes to how MIPS performance data should be captured for the upcoming performance year, it may be a relief to hear that largely the changes just build upon the existing 2017 regulations.
RELATED: A High-Level Overview of the 2018 MACRA Final Rule
Even though nothing too exceptional has been added, the amount of information can be overwhelming. With this in mind, here is an outline of the most important things to know for each performance category:
Cost
The most significant change to the MIPS performance categories is the inclusion of the Cost category in the MIPS final score. Previously, Cost has been tracked through administrative claims and MIPS eligible clinicians could view their performance feedback, but it did not affect their MIPS score at all.
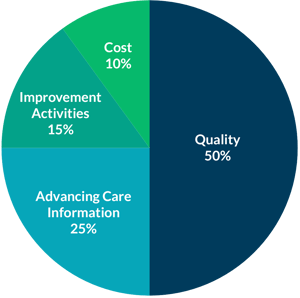
• Cost will be worth 10% of the 2018 MIPS Final Score.
• The performance period is the full calendar year (January 1, 2018-December 31, 2018)
• The Total per Capita Costs for all Attributed Beneficiaries measure and the Medicare Spending per Beneficiary (MSPB) measure will be used to determine your Cost category score in 2018.
• There were 10 episode-based measures that were used in 2017. However, those are not being used this year in favor of developing and gradually implementing new episode-based measures.
• Performance feedback for the two included measures and the episode-based measures in development will be available from CMS no later than July 1, 2018.
Quality
• Quality will be worth 50% of the 2018 MIPS Final Score.
• Instead of being able to opt for reporting for a 90-day period (as is the case for 2017 reporting), the performance period is the entire calendar year.
• The data completeness threshold is now 60% of all eligible visits for a measure.
• Clinicians and groups will be expected to report 6 quality measures, including one outcome measure (or a high-priority measure if an outcome measure is not available).
• Quality Measures data can be submitted via Claims, Qualified Registry, QCDR, CMS Web Interface, or EHR reporting.
• Scoring: Quality measures that meet the minimum case requirement, data completeness threshold, and have a benchmark will be worth between 3-10 points. If a measure has no benchmark or does not meet the minimum case requirement, it will only receive 3 points. If a measure does not meet the data completeness threshold, than only 1 point can be achieved, except for clinicians reporting from small practices (15 or fewer eligible clinicians).
Advancing Care Information
• ACI worth 25% of MIPS final score (unless participating in a MIPS APM).
• 2014 CEHRT will be acceptable for 2018, but bonus points will be given to those using 2015 CEHRT.
• Participants must still report the ACI base measures to receive any credit in this category at all. Successful base measure reporting must include one numerator instance where performance was met. Reporting base measures accounts for 50% of your ACI category points.
• The remaining 50% of ACI category points can be achieved through reporting numerator and denominator data for measure that have been specified as eligible or performance points.
• 10 bonus points will be awarded for reporting to any single public health agency or clinical data registry to meet any measures associated with the Public Health and Clinical Data Registry Reporting Objective / Public Health Reporting Objective. Additional registry participation will be worth 5 points.
• Certain Improvement Activities will qualify for 10 bonus points.
Improvement Activities
• Improvement Activities will be worth 15% of 2018 MIPS Final Score.
• Full credit in the Improvement Activities category is reporting 40 points worth of activities. Medium-weight activities are worth 10 points, and high-weight activities are worth 20 points.
• Clinicians practicing in rural areas, HPSAs, non-patient facing clinicians, and small groups only need to report for 20 points worth of activities. Self-identification requirement has been removed for 2018 and beyond.
• Submission Mechanisms through which you can attest to the completion of activities include via Qualified Registry, EHR, QCDR, CMS WI, or Attestation.
• Performance period is at least 90 days.
• The improvement activities inventory has been updated to include 21 new activities, 26 modified activities, and 1 removed activity.
• Clinicians participating in Patient-Centered Medical Home Models automatically get full credit for Improvement Activities. To be eligible for this, 50% of practice sites within the TIN must be recognized as a PFMH or similar model. A practice site is the physical place where services are delivered.
Too Much Information to Digest for Now?
Over the next few weeks, we will be releasing further summaries and fact sheets about the 2018 performance categories, available bonuses, MIPS final scoring, and participation in Advanced Alternative Payment Models. Subscribe to notifications to be alerted when these resources are available!

