ACOs have encountered challenges with aggregating, matching, and deduplicating extensive, disparate patient data required under the eCQM and MIPS CQM quality measure collection types. Patient matching and deduplication are needed to accurately calculate quality metrics from data across multiple practices and EHR instances.
Read on as we unravel the challenges and several methods to overcome these challenges.
Read More
Topics:
MACRA & MIPS,
MIPS CQMs,
MIPS Reporting
In the ever-evolving healthcare world, staying current is vital. Orthopedic surgery, particularly arthroplasty, has been at the forefront of the shift toward value-based care models. With certain procedures already subject to bundled payments for over a decade, the integration of cost measures within the Merit-Based Incentive Payment System (MIPS) is a game-changer.
Read on as we unravel the vital details of this essential aspect of modern healthcare performance assessment.
Read More
Topics:
MACRA & MIPS,
MIPS CQMs,
MIPS Reporting
With 2022 MIPS final scores available, hospitals and health systems have seen the Cost category produce a major impact on their overall MIPS scores.
Before CMS added the Cost category to 2022 MIPS scores, hospitals had little insight into how it would impact MIPS scores. With scores out, we see that many hospitals and health systems were scored on over 10 Cost category measures. That’s a large amount of data to sift through and analyze.
Read More
Topics:
MACRA & MIPS,
MIPS CQMs,
MIPS Reporting
Are you ready to jump back into the MIPS program?
The Centers for Medicare & Medicaid Services (CMS) have released Final Performance Feedback for the 2022 Merit-based Incentive Payment System (MIPS) performance period. We are seeing record maximum incentives of 8.25% for providers who achieved top scores.
Read More
Topics:
MACRA & MIPS,
MIPS CQMs,
MIPS Reporting
In the 2024 Proposed PFS Rule released in July 2023, CMS outlined a new option for MSSP participants to report quality measures called the Medicare CQM option. CMS created this reporting option to address concerns raised by ACOs and others, while still transitioning ACOs toward digital quality measure reporting.
Read on to learn more about the new proposed option for MSSP participants.
Read More
Topics:
MACRA & MIPS,
MIPS CQMs,
MIPS Reporting
With 2022 MIPS preliminary scores available, oncology practices are increasingly seeing how the Cost category negatively affects their overall MIPS scores.
Before CMS added the Cost category to 2022 MIPS scores, research hinted that oncology and other specialties with higher healthcare costs might face more adverse effects than other specialties. Numerous oncology practices opted for an Extreme and Uncontrollable Circumstances (EUC) exemption for the Cost category in 2022, mitigating the impact of cost measures on them.
Read on to learn more about how MIPS Cost scores are affecting Oncology practices.
Read More
Topics:
MACRA & MIPS,
MIPS Reporting,
MIPS Cost
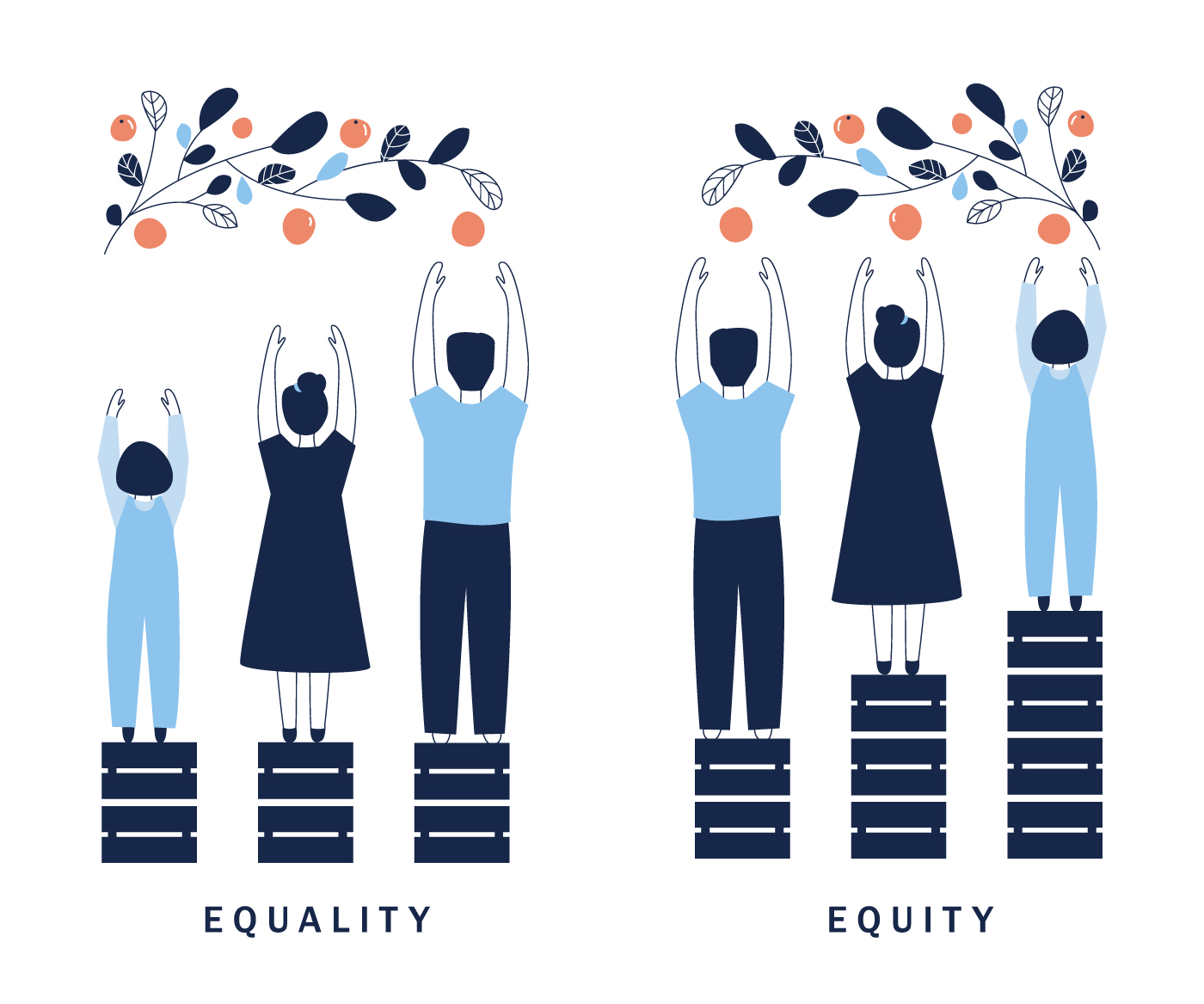
The 2023 Physician Fee Schedule (PFS) Final Rule was released in November 2022, finalizing many of the promised features of accountable care organizations (ACO) quality reporting. A couple weeks ago, I wrote about the Quality reporting requirements and Healthmonix's strategies to approach the upcoming changes. For Part 2 of this discussion, I will be introducing the new Health Equity Adjustment and why it will impact quality reporting moving forward.
Part 3 will cover the move from all or nothing scoring to a scaled approach.
Once again, if you are a visual learner, you can get most of this information from our latest webinar.
Read More
Topics:
MACRA & MIPS,
ACO,
APM Performance Pathway,
2022 PFS Final Rule,
Accountable Care Organization,
health equity,
Health Equity Adjustment
If you are a dermatology practice, you probably breathed a sigh of relief when the Centers for Medicare & Medicaid Services (CMS) announced that dermatologists, along with many other specialists, would no longer be attributed patients for the Total per Capita Cost (TPCC) measure, as part of the Cost component of the Merit-based Incentive Payment System (MIPS). However, in 2022, CMS introduced a Melanoma Resection Cost measure that is attributed to those specialists that perform these resections. So the Cost category is back for many dermatologists. Even if this is the only Cost measure that is attributed to your practice, it is worth 30 of your total 100 MIPS points - as much as all your Quality measures combined!
Read More
Topics:
MACRA & MIPS,
Cost Performance Category
As you report your MIPS data, it can feel like a lot of work with little ROI for the last two years. But wait. Sometimes we need to step back and evaluate the bigger picture. While we often focus on "getting the job done", there are changes in the healthcare economy that are occurring that are strategic.
Read More
Topics:
MACRA & MIPS,
APMs,
VBC,
Value-Based Care
On November 2, 2021, the Centers for Medicare & Medicaid Services (CMS) released the 2022 Physician Fee Schedule (PFS) Final Rule which governs MIPS and other quality payment programs. Anticipated changes were made to MIPS, making the program more challenging in 2022 and signaling additional changes to the program in coming years.
Read More
Topics:
MACRA & MIPS,
Quality Performance Category,
IA Performance Category,
Cost Performance Category,
PI Performance Category,
MIPS Value Pathways,
2022 PFS Final Rule

.png)
-3.png)
-4.png)