
The 2023 Physician Fee Schedule (PFS) Final Rule was released on November 6, 2023 and included over 3,000 pages of the Centers for Medicare & Medicaid Services (CMS) regulations and rulings for the 2023 year. While there is a ton of information to cover the entire rule, I would like to share what you need to know about the impact on the Medicare Shared Saving Program (MSSP) for Accountable Care Organizations (ACOs). In the first of this three-part series, I will cover Quality Reporting Requirements and Strategy. Subsequent blogs will cover Introduction to the Health Equity Adjustment and The Move from All or Nothing Scoring to a Scaled Approach .
If you are a visual learner, you can get most of this information from our latest webinar.
Quality Reporting Requirements and Strategy
CMS has solidified the path to the All-Payer reporting structure. They are providing ACOs ramp-up time before reporting eCQMs/MIPS CQMs become mandatory. There was no delaying the sunsetting of the CMS Web Interface. There was no reduction to what the proposed rule put forward regarding the path Quality reporting will take. In fact, any comment with regards to these changes was considered out of scope and met with no response.
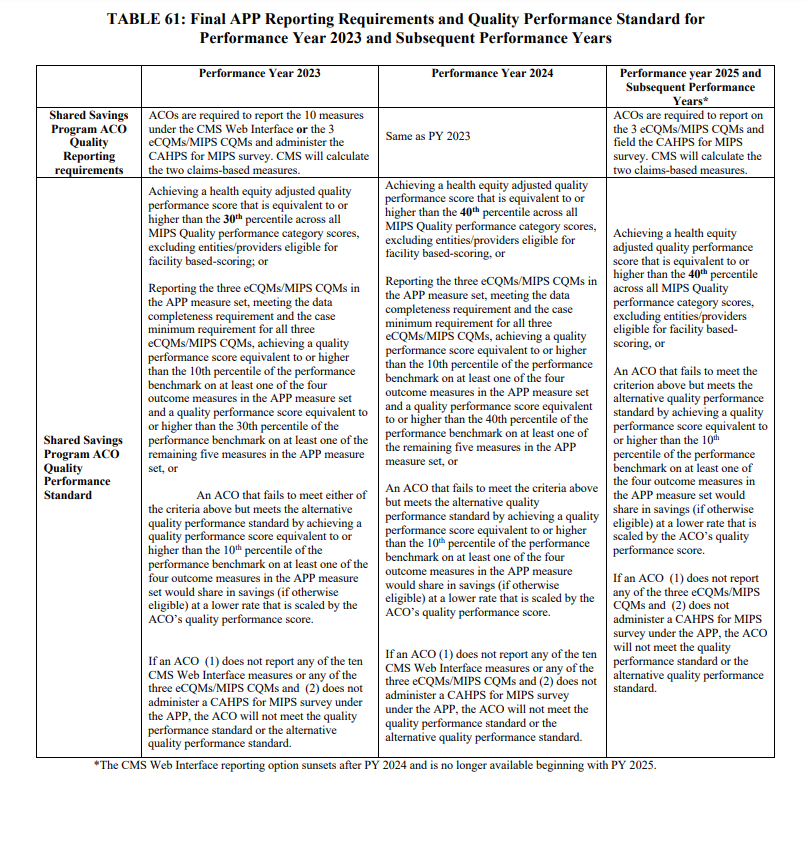
As you can see in table 61 below, CMS has laid out each of the options an ACO can take to report their quality measures for 2023, 2024, 2025 and subsequent years. There are advantages to getting started early with All-Payer reporting.
What exactly is All-Payer reporting and how does it work?
All-Payer reporting is a switch from a small subset of an ACO’s Medicare-attributed patients to all patients, for all ACO clinicians, independent of their insurance provider. CMS is seeking new processes to make healthcare more equitable across the entire US population, instead of just the Medicare population. While the idea overall sounds wonderful, ACOs are tasked with quite a challenge to comply with this requirement. Therefore, CMS is providing a timeline that allows ACOs to dip a toe in the waters starting now, before they must be fully compliant for PY 2025.
Our current clients and those ACOs we have spoken to over the last couple of months all seem to share the same anxieties.
- How do we get data from our aligned practices for non-Medicare patients?
- How do we combine data across multiple EHR platforms while reducing duplication?
- How do we do all of this and not negatively impact our clinicians and patients?
The work will not be easy and there can and will be struggles along the way, but CMS has outlined this process and provided you with the time to make incremental changes to your processes to limit impact. Our approach at Healthmonix considers the advantages of early adoption and the goal of being fully engaged prior to the mandatory changes in 2025.
Step 1 - PY 2023
- Identify all data sources for your ACO. Learn where each of your providers is documenting their quality information. Do they have an EHR? Are they utilizing separate billing software? Does the ACO have a data lake that captures all their data?
- Design and start the integration process. How will you gather all your data? Where will you store it? What vendors do you need to interact with? How often do you want to see results?
- Track and report CQMs AND the CMS Web Interface at the same time. CMS will take the best score between the two options. An ACO needs to reach the 10th percentile on one of the four outcome measures and the 30th percentile on any of the remaining five measures if you report CQMs in 2023.
- Work with clinicians to improve scores. Clinicians will need to be trained as they may have never needed to track these measures outside their Medicare population before. The hardest measure that we see clinicians having issues with is the depression screening measure. The population for this measure will be massive for most ACOs because it includes all patients 12 years and older who do not have a diagnosis of depression or bipolar disorder. The measure not only includes a screening being performed, but must also include a follow-up plan if the patient is positive. The hardest hit providers are going to be your specialists that are seeing patients who may not be seeing a primary care provider within your ACO.
Before we get into 2024 PY, I wanted to share a bit about what the differences are between an eCQM and a MIPS CQM. An eCQM is a measure that needs to be generated using certified electronic health record technology (CEHRT). The data collected for these measures are done through CMS published value sets that accurately capture patient data. The main benefit of an eCQM is the better benchmarks for higher scoring opportunities. CMS sets benchmarks for each measure based on the measure reporting type, and eCQMs have traditionally garnered lower scores. Therefore, groups that report eCQMs have a lower threshold to meet. However, the big hiccup to eCQMs is that clinicians will need to accurately document within their workflow to meet the measure specifications. If they do not document correctly, you cannot meet the measure.
A clinical quality measure (CQM) is like an eCQM in that it tracks quality data needed to report for the quality programs, but the main caveat is that a CQM does not need to be generated using CEHRT. Technically, a clinician may document CQMs on paper, on an Excel spreadsheet, or using a rock and chisel. The data must be backed up by the patient’s chart in case of an audit, but that is really the only rule. Reporting CQMs will provide ACOs the opportunity to submit data most accurately for the work that is being done by the clinician and their staff. Gaps in care can easily be overcome with chart reviews and will lead to a higher percentage of measure success. Ultimately, I believe that reporting CQMs early in the program adoption will lead to higher scores as the flexibility to reporting will outweigh the harder to reach benchmarks.
Step 2 – PY 2024
- Work with clinicians to accurately document measures to count for eCQMs. Now that you have driven successful CQM reporting, this is the time to start correcting data input to meet the goals of eCQMs. This may also include working with clinicians to upgrade EHRs to CEHRT or eliminating them from the ACO in the future.
- Refine data integration to stabilize the process. The program and scoring will get harder and having stabilized integration and data transfer will leave one area of concern out of the equation.
- Identify gaps in care. Utilize a system that allows you to attack your gaps in care by digging into your data to see where the needs are not being met. Are there certain clinicians not documenting correctly? Is there a measure that you are performing poorly in? Where can you make the biggest impact by changing behavior?
- Utilize data for non-MIPS related quality data. Now that you are collecting data for all the patients and visits your clinicians are seeing, you can start using it for more than just MIPS reporting. Track data for other value-based commercial plans that you participate in. Work with your local communities to establish better preventative care programs.
Step 3 – PY 2025
- Fully embrace eCQM tracking. Now that you need to achieve a Health Adjusted Quality Score equal to or higher than the 40th percentile, being able to report eCQMs will give you an advantage compared to the ACOs who are just starting. By this point, you should have trained your clinicians and staff on the proper way to document their notes to meet the measure standards. You can fully maximize your score by reporting eCQMs in full.
- Continue to drive performance improvement by utilizing the strategies that you have perfected during the ramp up period. You now have two plus years of experience with navigating the quality dashboards and understanding what trends are impacting your scores the most.
Last words
All-payer reporting is here. It is not coming. It is here. ACOs need to prepare now for when all-payer reporting is mandatory. The time to do that is now. There will be changes with reporting as this program matures and having your processes down now will allow you to pivot quickly. Healthmonix has the experience, expertise, and the ability to help you be successful. Our team is submitting both eCQMs and MIPS CQMs for multiple ACOs in 2022 already and have capabilities to incorporate your various technologies to maximize your scores and financial impacts.
Contact us today to learn how we can help.
