The NAACOS Fall 2021 Conference was the first live meeting that the Healthmonix team attended since HIMSS 2020 was cancelled in March of that year. It was certainly reinvigorating to meet in person, discuss the state of payment models, and hear from CMS regarding their vision.
Topics: CMS, ACO, Industry insights, 2021 PFS Proposed Rule
There has been much talk around MVPs in the CMS quality reporting arena. MVP means MIPS Value Pathway, and it’s a reporting framework that CMS is communicating as (a) the next evolution of MIPS and (b) a transition tool for getting to other alternative payment modules. As CMS continues to define and refine their vision of the MVPs, they have started to call the current framework 'traditional MIPS' to prepare for the inclusion of the MVP option. You’ll see this when you visit the QPP site. That said, how can MVPs affect MIPS?
Topics: MACRA & MIPS, CMS, 2021 PFS Proposed Rule, MIPS Value Pathways
MIPS 2021 Incentives and Penalties | How Can You Prepare?
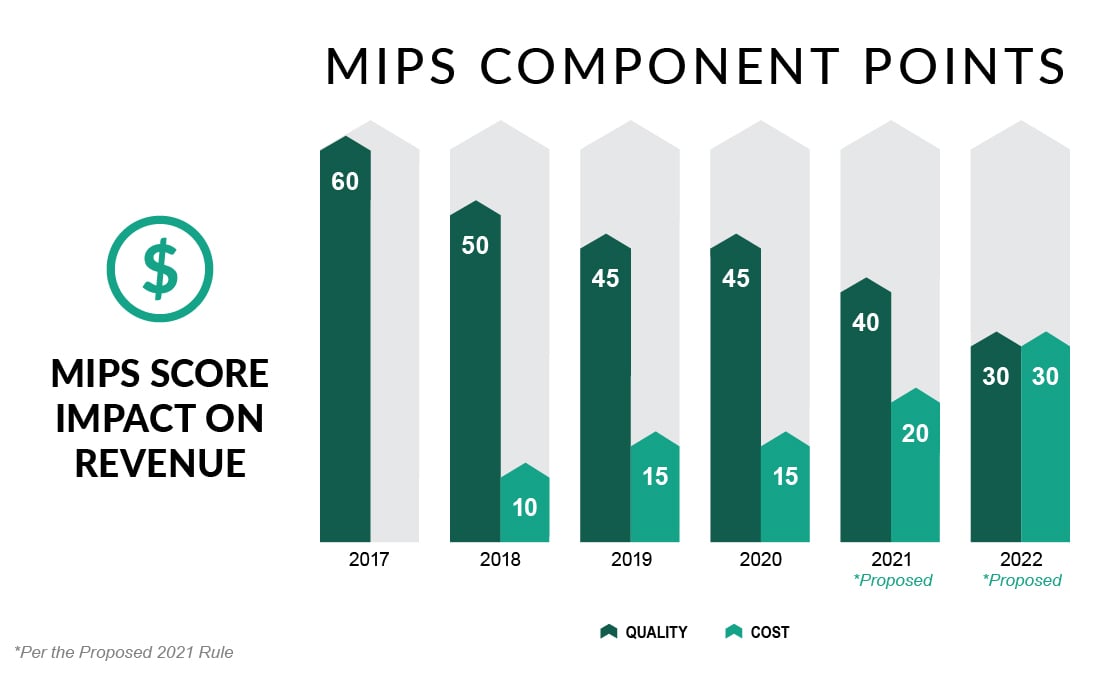
For years, we’ve heard that the Merit-based Incentive Payment System (MIPS) will provide a noticeable incentive for participants in this Medicare FFS program. And for years, there have been reasons why that has not occurred. First, CMS wanted to ‘start slow’ with the MIPS program in 2017 and 2018, so the caps on penalties and incentives were small. Then the potential penalties and incentives were raised, but the threshold for qualifying for an incentive remained low. This, coupled with the program’s budget neutrality meant there was not much revenue to distribute to high performers. Then COVID-19 negated much of the program for the last two years. So here we are, in year five, and we see that the program, for the first time, will have a significant downside and upside potential.
Topics: MACRA & MIPS, CMS, APMs, Cost Performance Category, 2021 PFS Final Rule
The 2021 Proposed Rule was released last week, and there are some potential changes that you should keep your eye on. Scouring through the entire release, it’s apparent that the Centers for Medicare & Medicaid Services (CMS) kept to their two main objectives:
- Minimize changes to reduce the burden on providers digging out of COVID-19
- Keep the momentum of the Quality Payment program moving forward
Topics: MACRA & MIPS, CMS, Policy, 2021 PFS Proposed Rule
The quick answer is NO!
There has been quite a bit of discussion, and some press, about the reporting period for MIPS for 2020. I have seen a few articles saying that no data reflecting services provided January 1, 2020 through June 30, 2020 will be used in the Center for Medicare & Medicaid Services (CMS’s) calculations for the Medicare quality reporting and value-based purchasing programs. However, if you read the Quality Payment Program – COVID-19 Response, Updated 6/24/2020, there is no mention of an all-inclusive change to the reporting period.
Topics: MACRA & MIPS, CMS, Industry insights
No CMS Updates on COVID-19's Impact on MIPS reporting - What it means
In the last couple of weeks, some major changes have been made to the immediate future of Value-Based Care payment models.
Some of these updates include:
- The extension of the Oncology Care Model (OCM) until June of 2022. The Centers for Medicare & Medicaid Services (CMS) is also giving practices the ability to abdicate downside and upside risk performance during the COVID-19 outbreak.
- The delay of starting the new Direct Contracting model to April 1st, 2021.
- The extension of the Next-Gen ACO model until December 2021.
- The option for participating entities in the Bundled Payments for Care Improvement Advanced (BPCI) payment model to eliminate upside or downside risk.
- The removal of COVID-19 episodes of care for certain Medicare ACO models.
Topics: MACRA & MIPS, CMS, COVID-19
CMS relaxes more rules around telehealth, allowing healthcare across state lines
The Centers for Medicare & Medicaid Services (CMS) continues to relax regulations to enable hospitals, clinics and other providers to boost their front-line medical staff during the COVID-19 pandemic. This pandemic has created an urgency for expansion of the use of virtual healthcare to reduce the risk of spreading the virus. It has also created a need to relax practice restrictions and allow more flexible care practices to meet the needs of patients.
Topics: CMS, Interoperability, Industry insights, Policy, Health IT, VBC, COVID-19
Between 2018 and 2019, 74 of Medicare’s 561 accountable care organizations (ACOs)—or 13%—left the program, according to research by Leavitt Partners. The same research also found that 26% of ACOs that reached the end of their three-year agreement opted to not renew it at the end of 2018.
New CMS Toolkit: 5 Care Coordination Strategies For ACO Success
A new CMS toolkit, released through the CMS ACO learning system, shows five innovative care coordination strategies that have helped Medicare ACOs find success through shared savings.
CMS To Launch New Payment Models For Value-Based Transformation
On April 22, the U.S. Department of Health and Human Services (HHS) and Centers for Medicare & Medicaid Services (CMS) announced the CMS Primary Cares Initiative, a new set of payment models that are part of HHS Secretary Alex Azar’s value-based transformation initiative. The CMS Primary Cares Initiative will be administered through the CMS Innovation Center. CMS expects the new programs to shift at least one quarter of people in traditional Medicare out of fee-for-service.