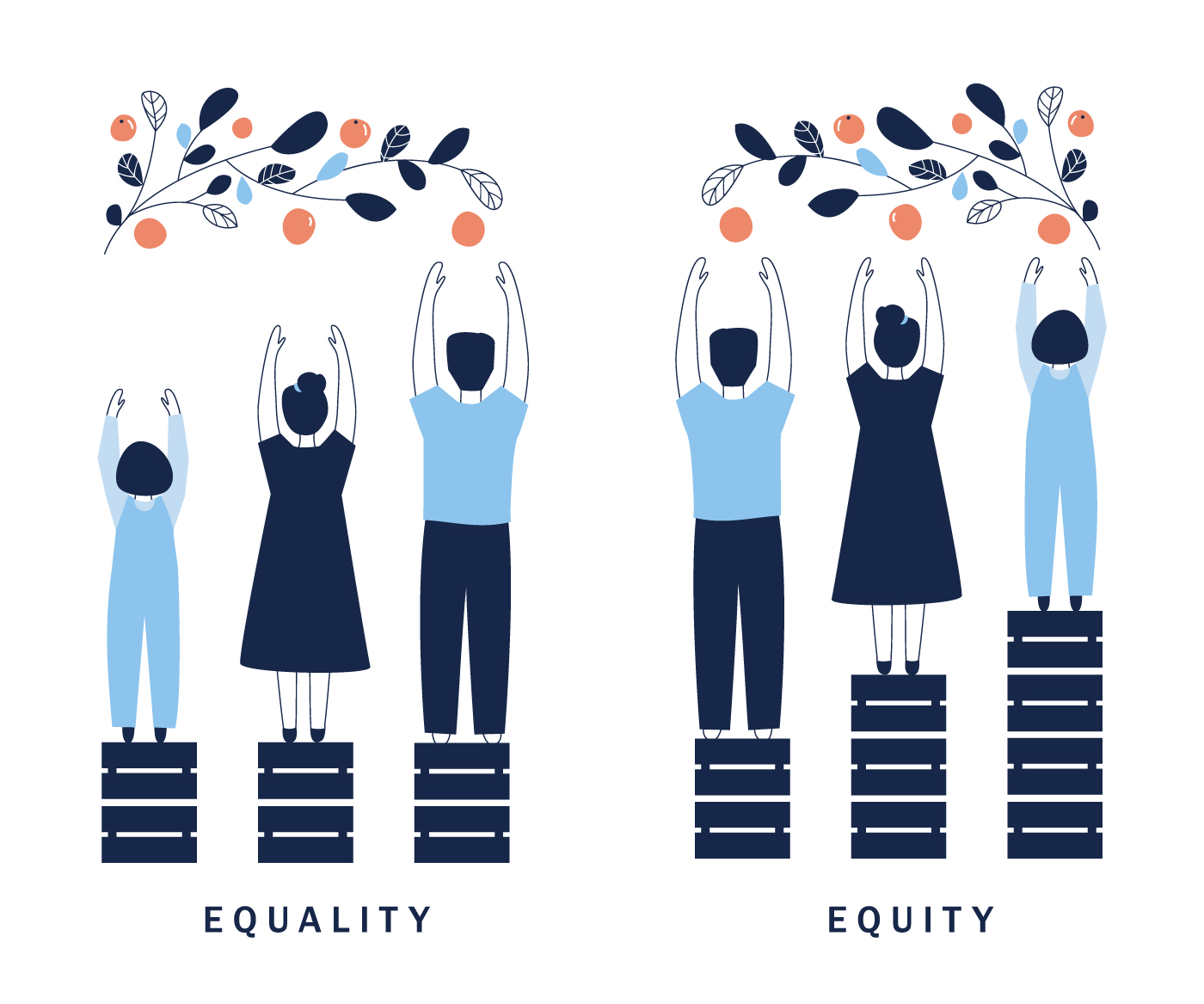
The 2023 Physician Fee Schedule (PFS) Final Rule was released in November 2022, finalizing many of the promised features of accountable care organizations (ACO) quality reporting. A couple weeks ago, I wrote about the Quality reporting requirements and Healthmonix's strategies to approach the upcoming changes. For Part 2 of this discussion, I will be introducing the new Health Equity Adjustment and why it will impact quality reporting moving forward.
Part 3 will cover the move from all or nothing scoring to a scaled approach.
Once again, if you are a visual learner, you can get most of this information from our latest webinar.
Read More
Topics:
MACRA & MIPS,
ACO,
APM Performance Pathway,
2022 PFS Final Rule,
Accountable Care Organization,
health equity,
Health Equity Adjustment
The 2023 Physician Fee Schedule (PFS) Final Rule was released on November 6, 2023 and included over 3,000 pages of the Centers for Medicare & Medicaid Services (CMS) regulations and rulings for the 2023 year. While there is a ton of information to cover the entire rule, I would like to share what you need to know about the impact on the Medicare Shared Saving Program (MSSP) for Accountable Care Organizations (ACOs). In the first of this three-part series, I will cover Quality Reporting Requirements and Strategy. Subsequent blogs will cover Introduction to the Health Equity Adjustment and The Move from All or Nothing Scoring to a Scaled Approach .
If you are a visual learner, you can get most of this information from our latest webinar.
Read More
Topics:
ACO,
APM Performance Pathway,
Medicare Shared Savings Program,
Accountable Care Organization,
MIPS CQMs,
eCQMs,
2015 Edition CEHRT,
certified electronic health record technology,
2015,
2023 PFS Final Rule
If you are managing a Medicare Shared Savings Program accountable care organization (MSSP ACO), you have heard the mandate from the Centers for Medicare & Medicaid Services (CMS) to move to eCQM/CQM reporting, replacing the Web Interface reporting. You may also be aware of the significant pushback that ACOs, collectively and independently, have provided to CMS. At this year’s fall National Association of ACOs (NAACOS) conference, the tenor changed to accepting the move, optional in 2022 through 2024, but required in 2025.
Read More
Topics:
ACO,
APM Performance Pathway,
Accountable Care Organization,
MIPS CQMs,
eCQMs
The 2023 Provider Fee Schedule Proposed Rule was released in July and there are changes that accountable care organizations (ACOs) need to be aware of. This blog will focus on the most important changes from a quality reporting perspective.
Read More
Topics:
ACO,
APM Performance Pathway,
2023 Proposed Rule,
health equity
For ACOs participating in the Medicare Shared Savings Program (MSSP), CMS is implementing rules in 2021 and 2022 for quality reporting which include a sweeping change. This change will require a new reporting approach, in order to aggregate data from electronic health record systems used across an ACO for all patients seen by any provider, regardless of payer or participation in the ACO. In a recent survey, nearly 75% of the ACO respondents indicated concern with the challenge of these requirements. The Web Interface reporting is being sunset, and ACOs need to devote attention to determining their strategy for transitioning quality reporting. Success will require thoughtful planning and experienced system implementation.
Read More
Topics:
ACO,
APM Performance Pathway,
Medicare Shared Savings Program
As we move into 2021 and beyond, we see CMS putting some real teeth into the Merit-based Incentive Payment System (MIPS) program. This is the first year where we see more than two percent incentives possible. Exemptions and exclusions are narrowing. Participants in other value-based programs are being forced into MIPS reporting because of higher thresholds for exclusion and elimination of other reporting options.
Read More
Topics:
MACRA & MIPS,
MIPS Value Pathways,
APM Performance Pathway
The long-awaited CY 2021 Medicare Physician Fee Schedule Final Rule update is now here. Despite the disruptions of the Public Health Emergency COVID-19, participation in performance year 2019 was strong. Thus the 2021 Final Rule moved forward with finalizing a number of proposed changes, including a higher performance threshold for performance year 2021, anticipated changes in weight to the Quality and Cost performance categories of the Merit-based Incentive Payment System (MIPS), and the introduction of the APM Performance Pathway. Other expected initiatives, such as MIPS Value Pathways, the requirement for registries to build their own benchmarks for certain measures, and the sunsetting of the CMS Web Interface, have been pushed back to at least the 2022 performance year.
Read More
Topics:
MACRA & MIPS,
APMs,
COVID-19,
2021 PFS Proposed Rule,
APM Performance Pathway