The 2023 Provider Fee Schedule Proposed Rule was released in July and there are changes that accountable care organizations (ACOs) need to be aware of. This blog will focus on the most important changes from a quality reporting perspective.

Health equity has become the newest initiative that the Centers for Medicare & Medicaid Services (CMS) is incorporating in ACO requirements. This change to eCQM/MIPS CQM measures was highlighted in the Proposed Rule, and more details will emerge. As many ACOs are beginning to prioritize finding solutions that tackle the difficult task of reporting eCQM/MIPS CQMs through the APM Performance Pathway requirements, the new health equity focus adds another layer of complexity to this effort.
Many ACOs have stated that, as quality performance standards are increased, the “all-or-nothing” approach to scoring can have a dramatic, negative impact on their reimbursement. CMS heard this concern and is now proposing for the 2023 performance year, that there will be a sliding scale scoring for the quality performance standard. This will align with the current MIPS scoring where ACOs will not be penalized greatly for just missing the marks. Flexibility is the key factor as the move to eCQM/MIPS CQM measure reporting becomes mandatory.
CMS is adamant that ACOs need to start reporting on all patients and all measures by the 2025 performance year. There were no indications that this plan will be adjusted in the Proposed Rule. CMS understands the hardship that this will cause for ACOs and is providing them opportunities through a ramp-up process that will provide them flexibility in 2023 and 2024.
In the chart below you can see differences in the responsibilities during the ramp-up period compared to the 2025 performance year.
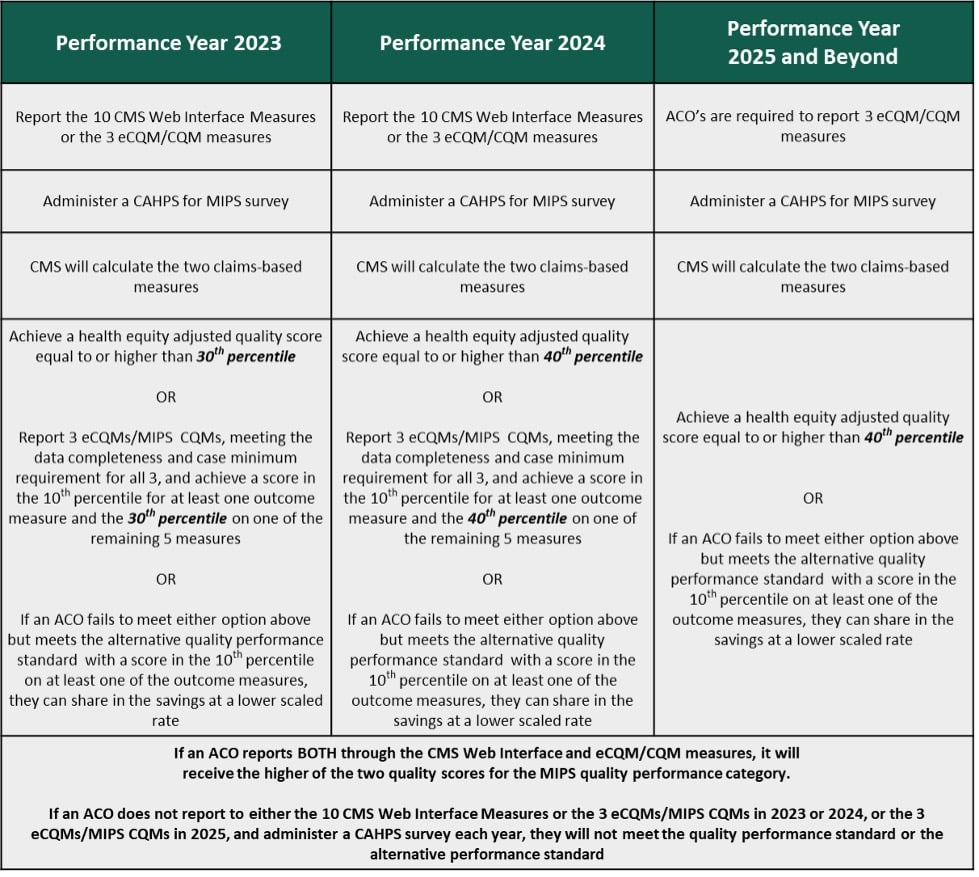
For the 2023 and 2024 performance years, the CMS Web Interface is still an option for reporting your quality measures, however CMS is incentivizing ACOs to move toward with eCQM/MIPS CQM reporting. To meet the quality standards for 2023, there are additional options in lieu of the Web Interface. ACOs will be able to meet those requirements by achieving a health equity adjusted quality score equal to or higher than the 30th percentile, or report on three eCQMs/MIPS CQMs and achieving a score in the 10th percentile for at least one outcome measure and the 30th percentile for one of the remaining five measures. If an ACO fails to meet either of those options, but meets the alternative quality standard for at least one outcome measure in the 10th percentile, they will be eligible to share in the savings at a lower scaled rate.
So, how does CMS plan to track “health equity”? First, let's take a step back and discuss why health equity is imperative to the quality programs. By adding all payers to the quality reporting programs, CMS is introducing a patient population that is currently being underserved by the health industry. The uninsured and Medicaid populations tend to have lower quality scores due to many factors including income, education, environment and access to health care to name a few. The idea is not to have everyone receive the same benefits of this program, but to have the same access to health care as a whole.
To make the adjustment for health equity, CMS is proposing a complicated equation to score each ACO on their quality performance.
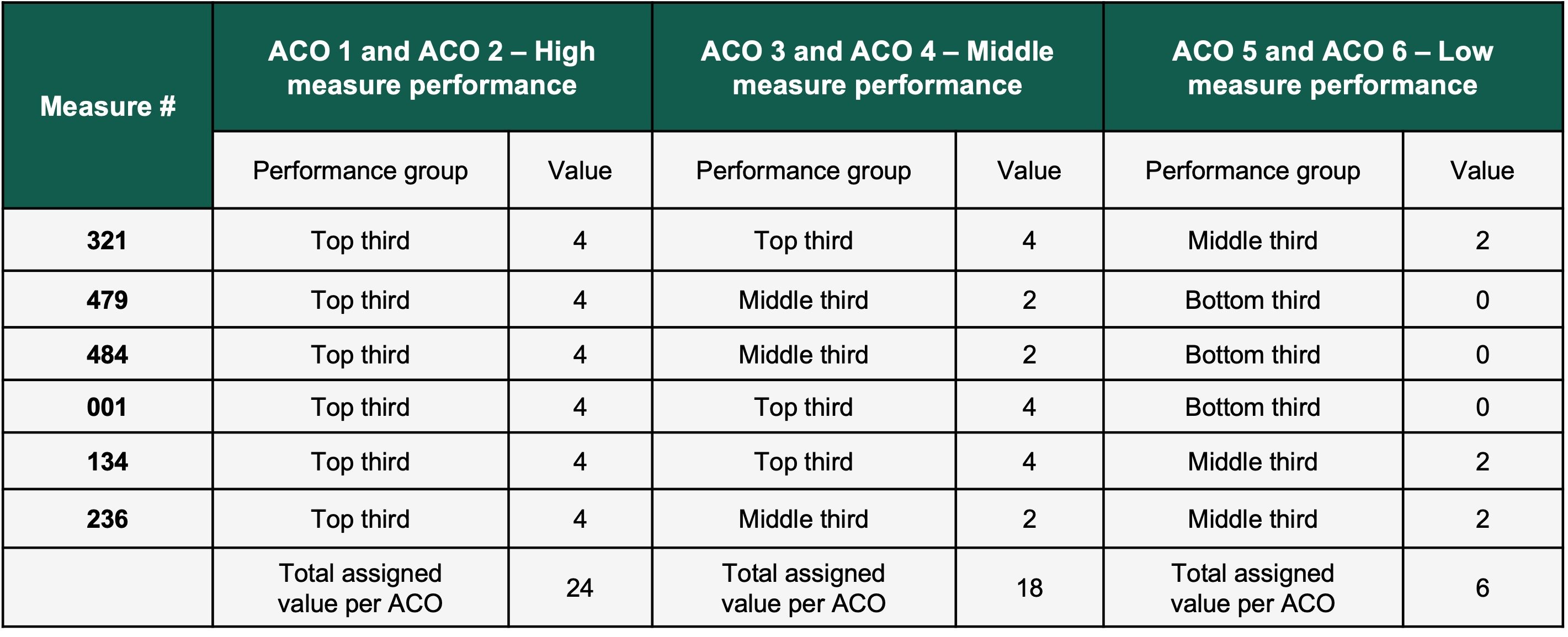
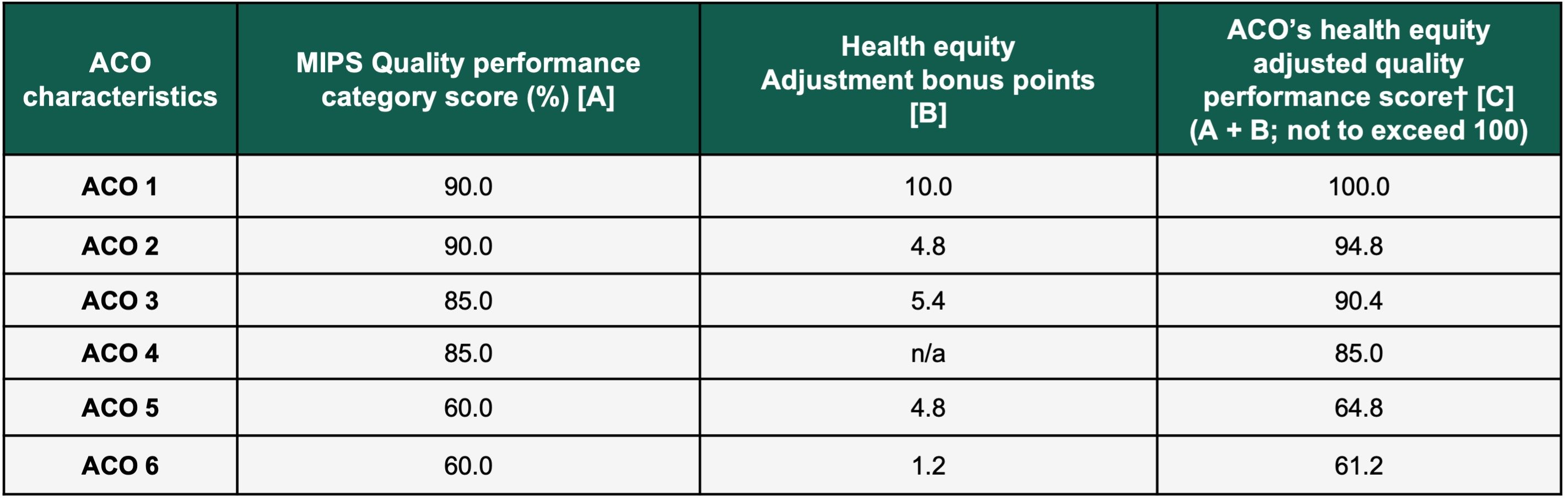
The following charts from the 2023 Proposed Rule will walk you through the process that is being recommended:
The first step will provide an individual score for each quality measure. Each measure will be given a value based on their performance, such as top third of performers (four points), middle third of performers (two points), and bottom third of performers (zero points). The maximum number of points earned will be 24 (six measures X four points).
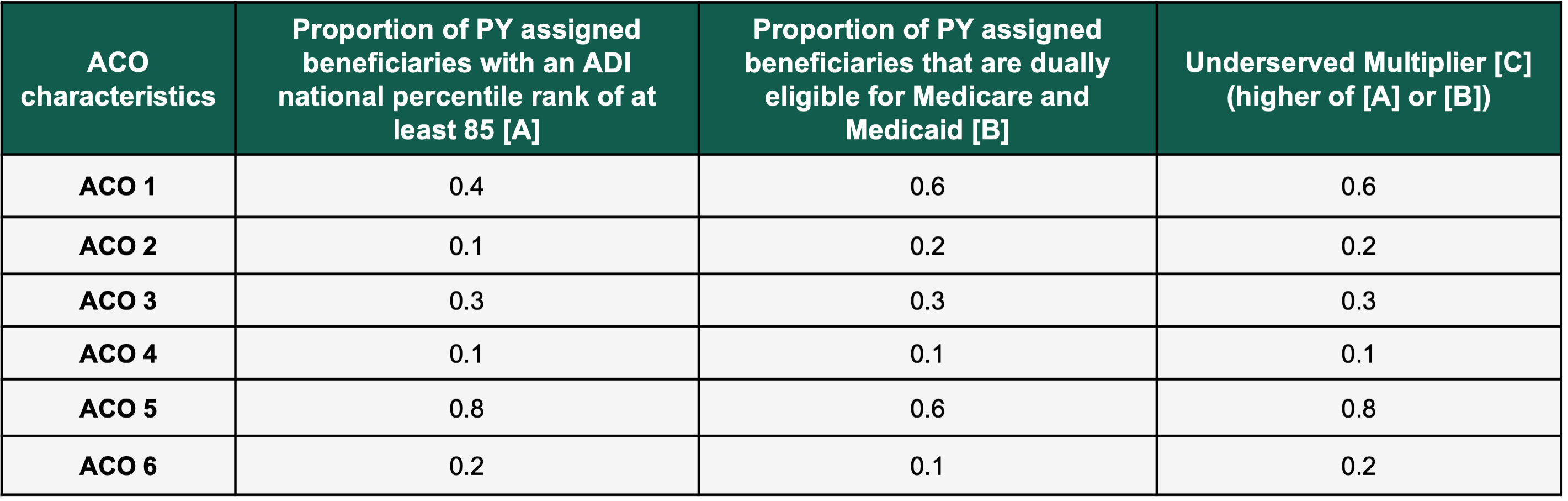
Step two will calculate the underserved multiplier that will be used in the equation. It will take the greater of the two scores between the proportion of performance year assigned beneficiaries with an ADI (Area Deprivation Index) national percentile rank of at least 85, and the proportion of performance year assigned beneficiaries that are dually eligible for Medicare and Medicaid.
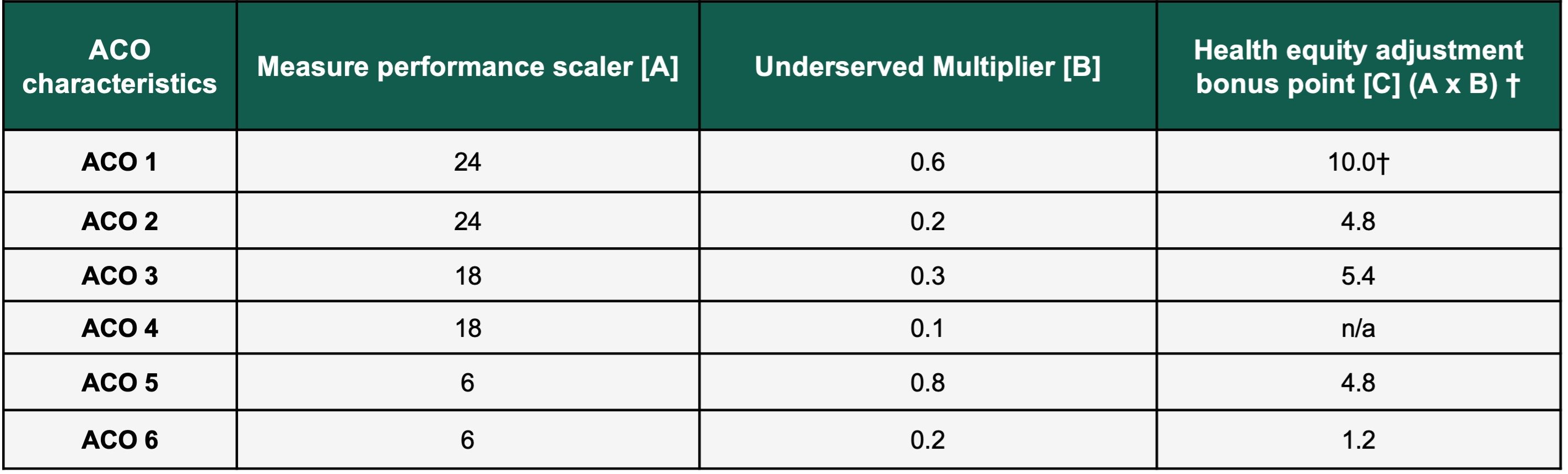
Step three will combine steps one and two to create a health equity adjustment score. The maximum adjustment points that can be awarded is 10. An ACO that does not meet the minimum percentage of underserved individuals will not be awarded any bonus points.
Step four, the final step, will now take the overall MIPS Quality performance score and add the health equity adjustment score. This will result in the overall ACO’s health equity adjusted quality performance score.
Clearly CMS is looking to reward high quality ACOs that adopt the new eCQM/MIPS CQM scoring methodologies. Both the health equity bonus and the reduced quality score requirements should motivate ACOs to adopt the new reporting processes in 2023. The influx of calls and inquiries to my team since the Proposed Rule was released verifies to me that ACOs are now taking the eCQM/MIPS CQM reporting transition seriously. There is still a long way to go for CMS to make actual patient level health equity impact, but this could be the beginning that we think most healthcare organizations can get behind.
The message is clear from CMS. Health equity is an important way for ACOs to track and adjust their patient care. The incentives to move towards these two goals will only be here for the next two years. Those organizations that wait until 2025 to adopt these methodologies will be well behind their peers. The process can be overwhelming, but having a partner like Healthmonix to lead you down the path will enable your ACO to succeed at eCQM/MIPS CQM reporting and continue to see shared savings.
Please feel free to reach out to me to start the discussion today.
Steven Tyson
215-330-5254
