With the beginning of June came the half-way point for the first year of MIPS reporting. While many providers haven't started reporting yet, a good number of clinicians have started early. We interviewed clinicians and practice administrators who have reported PQRS in the past via registry, are currently reporting through the MIPSPRO registry, and that represent a diverse demographic of MIPS eligible clinicians.
Topics: PQRS, MACRA & MIPS, Industry insights, Small Practice, Hospitals & Health Systems
In December we posted about a CMS announcement related to ICD-10 diagnosis and procedure code changes, and how this might affect payment adjustments in 2018. At the time CMS had not yet issued their addendum detailing specific code updates for measures being used in the Merit-Based Incentive Payment System (MIPS), but now that they have, here’s an update:
CMS and the National Library of Medicine (NLM) have published the addendum to the 2016 eCQM specifications which affects ICD-10 Clinical Modification (CM) and Procedure Coding System (PCS) value sets for 2017. Health Quality Measure Format (HQMF) specifications, value set object identifiers (OIDs), and measure version numbers for 2017 were not changed. The eCQM value set addendum for 2017 is published to the eCQM Library and the eCQI Resource Center. The NLM’s Value Set Authority Center also provides a complete list of revisions to the eCQM value sets.
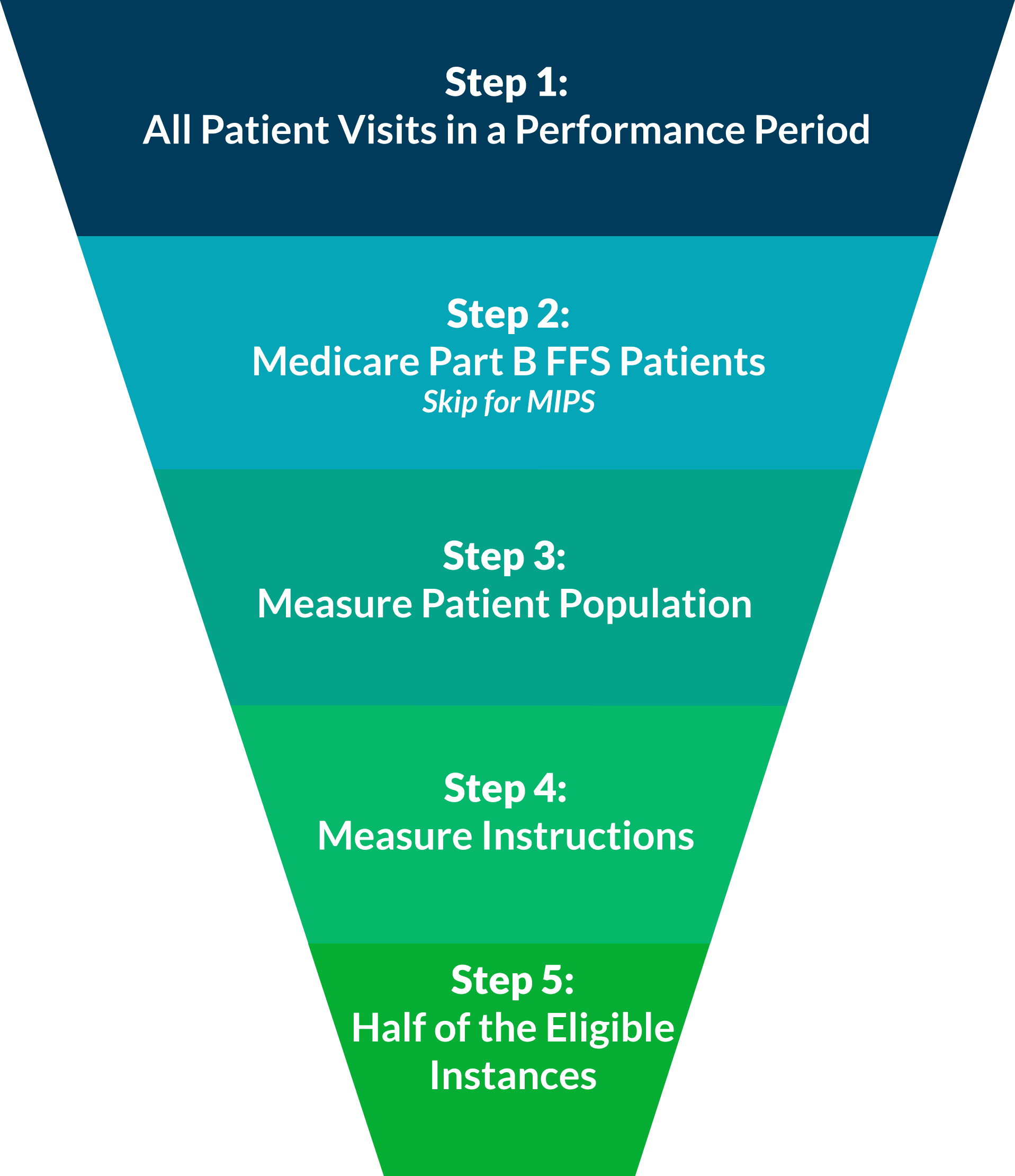
When reporting individual quality measures, whether it be for PQRS this year, or for one of the performance categories of MIPS next year, you are expected to report at least 50% of your eligible instances for each measure. In our experience, this concept can be confusing when practically applied. Luckily, it can be disambigusted in five easy steps!
Consider All Patient Visits for the Performance Period
A performance period for PQRS is based on a complete calendar year beginning on January 1 and ending on December 31.
For MIPS reporting, the performance period can range from a continuous 90-day period to the full calendar year.
Last night, a very surprising article was promoted, "CMS waves Physician Quality Reporting System penalties for 2017, 2018 after massive ICD-10 update clogs system." This post makes it seem as if only the Value-Based Modifier (VM) program penalties and incentives would still be in effect based on PQRS reporting done in 2015 and 2016. This is a dangerous misconception.
Once you've selected how you will report, the next step is to determine what you will report. This is called your reporting method. You have two options: reporting a measures group or reporting individual measures.
Last week, we discussed the first step to reporting PQRS in 2016, selecting a submission mechanism. To briefly recap, there are three submission mechanisms that are viable for practices starting to report at this point in the year: Registry, EHR, and QCDR. Of these three options, Registry reporting has the highest rate of success and ease of submission.
We call it “Informal Review Season”. You could also call it “the Nightmare Vaguely Before Christmas” for
providers who bill Medicare Part B services. The 2015 PQRS Informal Review season (this year September 26th through November 30th) is that most wonderful time of the year when practitioners and practice administrators nervously await the release of feedback reports in September. Instead of children wondering whether or not they’ve made Santa’s list, you’ve got providers and practitioners feverishly paging through their QRURs to see exactly how naughty or nice they are, according to CMS. (Note: Documents released in the fall of 2016 pertain to the 2015 PQRS or VBM reporting period).
Topics: PQRS
Reporting PQRS in 2016 is just as important as ever, with up to 6% of your Medicare Part B reimbursements on the line in 2018. According to the latest PQRS experience report[1], about 66% of eligible providers are participating in PQRS. Of these participating providers, 68% are still reporting using the claims-based reporting mechanism, which has an abysmal 40% success rate in avoiding the PQRS penalty. Just taking these numbers into account, this takes us up to at least 61% of PQRS eligible providers not avoiding the PQRS penalty.
10 PRO Tips for Conquering the Quality Performance Category of MIPS (Part 2)
Last week, we introduced some of the core concepts of the MIPS Quality Performance Category. This week, we are going to elaborate on these premises with Part 2 of our "10 PRO tips for Conquering the Quality Performance Category of MIPS."
Topics: PRO Tips, PQRS, MACRA & MIPS, Quality Performance Category
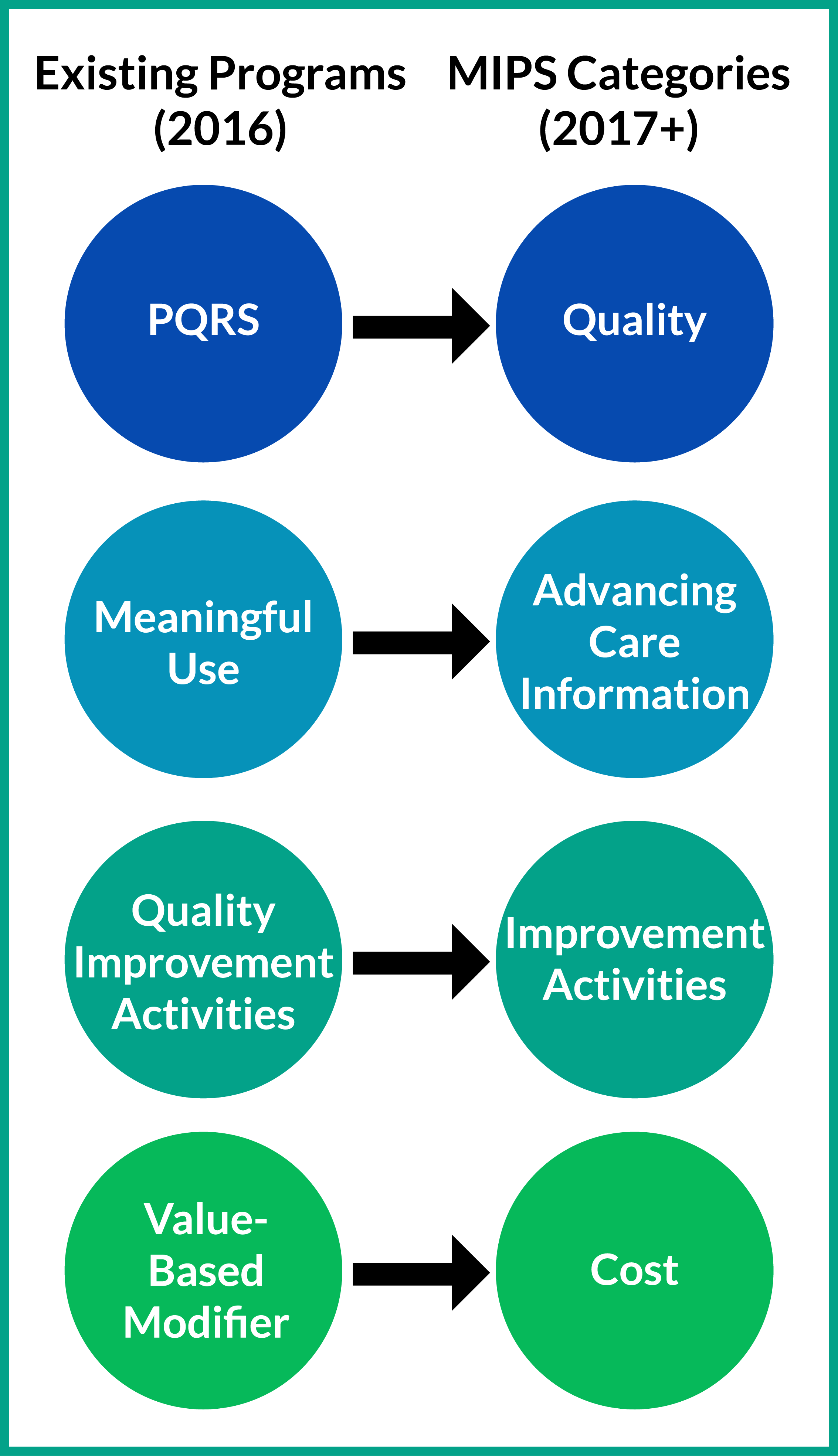
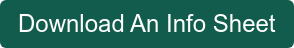
The Four Performance Categories of MIPS: PQRS in Sheep's Clothing
As a young adult from a small town in Ohio, the prospect of leaving my hometown to go to college was a frightening one. I was anxious to leave the familiarity of my high school, and the routine I had perfected to remain an A student. The only expectation that I had was given to me by my teachers, who reported that college would be significantly different and more challenging than high school. As I packed up my ‘63 International Scout to drive to college in August of 1975, the fear of failure was present and strong. However, when I arrived, I found the classes were similar, the pedagogical approach was the same, and as long as I showed up and did the work, I could do as well as I did in high school.
Topics: PQRS, MACRA & MIPS, Policy, Quality Performance Category, ACI Performance Category, IA Performance Category, Cost Performance Category