Under the forthcoming Medicare Access and CHIP Reauthorization Act (MACRA), the Physician Quality Reporting System (PQRS) is being absorbed into the Merit-Based Incentive Payment System (MIPS). Specifically, PQRS will transition into one of the four Performance Categorys of MIPS, the Quality Performance Category.
To help MIPS Eligible Clinicians prepare now to maximize their revenue under MACRA's MIPS, we have compiled a list of Performance Reporting Optimization Tips, or PRO Tips about the Quality Performance Category of MIPS. Previously, we have compiled PRO Tips for the Advancing Care Information Performance Category of MIPS. Additionally, we have forthcoming articles detailing PRO tips for the Clinical Practice Improvement Activity (CPIA) Performance Category and the Resource Use Performance Category.
![]()
The Quality Performance Category is worth HALF of your MIPS Composite Performance Score (CPS).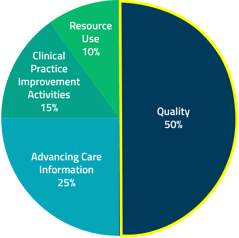
Each of the four MIPS Performance Categorys will be weighted differently to add up to your MIPS CPS. Of the four MIPS Performance Categorys, the Quality Performance Category is weighted the heaviest for year one of MIPS at 50% of your total MIPS CPS.
Since the Quality Performance Category is worth half of the MIPS CPS, if you are looking for one Performance Category to really focus on perfecting for the first performance period, Quality is definitely the Performance Category to choose.
 The process of reporting will not change significantly from the way it is currently being handled through PQRS reporting.
The process of reporting will not change significantly from the way it is currently being handled through PQRS reporting.
Like with PQRS, you will have the option to choose the mechanism through which you report (e.g., registry reporting, through an EHR, or GPRO web interface). Additionally, you will have the option of reporting individually or as a group, and will be expected to report similar quality measures. However, the scoring and impact of reporting is proposed to change immensely. No longer is it a Pass / Fail system where completion of reporting meets the success criteria for the eligible provider (EP), but the impact of reporting will be scaled based upon the reported performance metrics.
 The number of required measures to report has been decreased, but measures group reporting is also being retired.
The number of required measures to report has been decreased, but measures group reporting is also being retired.
You will have to select 6 measures, including at least one outcome (or high priority) measure and one cross cutting measure from the master measures list or from the specialty-specific measure lists (Table A and E respectively in the appendix to the proposed rule). (Note: that lists are provided for only 23 specialties; all other specialties must select from the master measures list.)
For each measure, compute your performance score based on at least 90% of your entire patient population.
 Unlike PQRS, achievement within the Quality Performance Category will be expressed in a performance score, rather than by pass / fail.
Unlike PQRS, achievement within the Quality Performance Category will be expressed in a performance score, rather than by pass / fail.
To determine your Quality Performance Category performance score, you must first determine your performance score for each measure. For the performance score on each measure, compare the score to the national benchmark and earn up to 10 points depending on which decile your performance score falls in. For example, if the score is in the 50% percentile, you will earn 5 points for reporting that quality measure.
Then, add the scores for all measures reported. add in additional points for:
- Two bonus points for reporting each extra outcome measure beyond the one required
- Two bonus points for reporting the patient experience measure (CAHPS for MIPS survey counts as one patient experience measure)
- One bonus point for reporting each extra high priority measure
- One bonus point for each measure reported using CEHRT in end-to-end reporting
- Scores for two or three additional measures will be calculated by CMS based on claims data. (acute composite, chronic composite, readmissions)
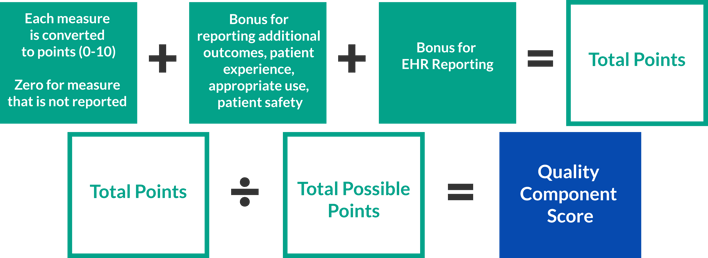
Once that score is calculated (complicated, I know!), only then will you know where you sit in terms of total points. There are a total of 80 or 90 available (depending upon the size of your practice), and your total out will be what is compared then to all eligible professionals (EPs) to determine where you fall in the incentive / penalty scale.

Under the Quality Performance Category of MIPS, achieving a significant incentive is possible again.
Based upon 2016’s Value-Based Payment data, we should be looking for rather large payment increases for high performers under the MIPS program. This year there were very few high performers (128 groups to be exact) but a significant number of non-reporters (over 5,000 groups). That means that the money CMS collected in penalties from the non-reporters went to a small cohort of high-performers, driving bonuses to upwards of 15%. That bonus potential gets pretty steep in 2022 at 27%. However, we believe that payment increases will not be this steep. By 2022, more providers will have invested in quality reporting. Fewer non-reporting providers means less penalty money to divvy up among high performers.
Next week, we will conclude this list with Part 2 of "10 PRO Tips for Conquering the Quality Performance Category of MACRA's MIPS. For now, the number one PRO tip we can give you is really to start monitoring and reporting PQRS measures. Note your performance scores, compare to national benchmarks (available within PQRSPRO), and determine if there are areas of improvement to consider.



 The process of reporting will not change significantly from the way it is currently being handled through PQRS reporting.
The process of reporting will not change significantly from the way it is currently being handled through PQRS reporting. Unlike PQRS, achievement within the Quality Performance Category will be expressed in a performance score, rather than by pass / fail.
Unlike PQRS, achievement within the Quality Performance Category will be expressed in a performance score, rather than by pass / fail.