Why MIPS 2020 Will Be More Difficult Than Keeping a New Year’s Resolution
Topics: PRO Tips, MACRA & MIPS, Policy, Healthmonix, Eligibility
Last Minute Hacks for Small Group MIPS 2019 Reporting
Topics: PRO Tips, Policy, Healthmonix, Eligibility
MIPS Hacking for Psychologists: Turbo-boost your ROI With This One Simple Trick.
In last week’s blog I laid out the case for opting into MIPS, an option that allows clinicians and groups to still receive a MIPS payment adjustment if they exceed 1 or 2, but not all, elements of the low-volume threshold. Although this option can be beneficial for a wide range of clinician types depending on their situation, today I want to focus on psychologists in particular. Because in my experience, they provide some of the most striking examples of this “MIPS hack” in action.
Topics: PRO Tips, MACRA & MIPS, Eligibility, Small Practice, VBC, ROI
MIPS Hacking: Why the MIPS Opt-In Policy Could Seriously Boost Your Bottom Line.
Beginning in 2019, otherwise-eligible clinicians, groups, and APM entities can elect to opt-in to MIPS if they exceed 1 or 2, but not all, elements of the low-volume threshold. That means that for the first time, these previously ineligible clinicians have the opportunity to participate in the QPP and earn a payment adjustment.
Now maybe you haven’t had the time to pay close attention to policy minutiae, and this is the first you’re hearing of the opt-in option. Or maybe you’ve heard of it, but haven’t looked seriously at what it could mean for you or your organization. After all, on the surface it just sounds like work that isn’t required--and could it really make enough of a difference to your bottom line to be worth it?
Well, we highly recommend you do the math to find out. Because depending on your situation, you might be very, very glad you did.
Topics: PRO Tips, MACRA & MIPS, Eligibility, Small Practice, VBC, ROI
Your One-Stop Guide To Understanding QP and Partial QP Determinations in 2019
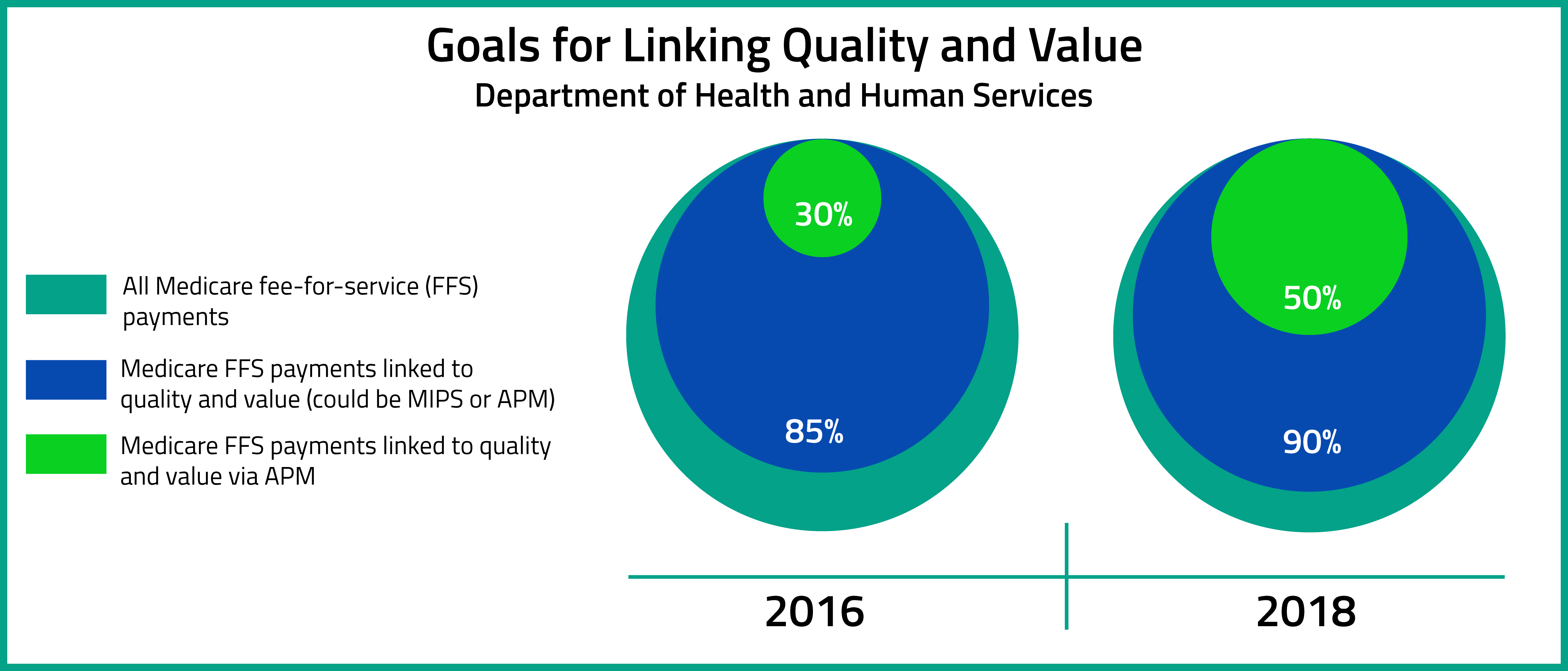
When the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) was signed into law, it created two distinct pathways for reporting: the Merit-Based Incentive Payment System (MIPS), and the Advanced Alternative Payment Model (Advanced APM). Under MIPS, Medicare Part B payments are tied directly to clinician performance based on Composite Performance Scores (CPS), whereas the Advanced APM track encourages groups of clinicians to take on greater risk (and reward) for cost and quality of care.
In this week’s blog, we’re taking a deep dive into Qualifying APM Participant (QP) and Partial QP Determinations, as laid out in the 2019 QPP final rule.
Topics: Policy, Eligibility, APMs
To Do: Check Your MIPS Eligibility Status, Preview Your QPP Data.
Have you checked your 2018 MIPS eligibility status? Since September?
CMS emailed physicians to let them know that their MIPS status for this year may have changed that recently--and some physicians may find that they are no longer eligible to participate. Although CMS conducted an initial review of Medicare Part B claims and Provider Enrollment, Chain, and Ownership System (PECOS) data between September 2016 and August 2017, further updates were made after a second review that took place between September 2017 and August 2018. If you are eligible, your 2018 performance will affect your 2020 Medicare payment adjustment.
Topics: PRO Tips, MACRA & MIPS, Eligibility
Three Ways to Check Your MIPS Participation Eligibility Status
When we asked MIPS eligible clinicians about their experiences transitioning from PQRS this year, one of the biggest takeaways was that quality matters even more under MIPS than it did under PQRS. Clinicians who want to maximize their reimbursement would consequently be very smart to start reporting as early as possible, and to adjust performance to maximize quality, rather than waiting until the end of the year. If you’re not sure whether or not you are a MIPS-eligible clinician, take advantage of one of the following resources for determining your MIPS participation status as soon as possible so that you don’t get left behind.
Topics: PRO Tips, MACRA & MIPS, Eligibility
We are now in the seventh month of the new Merit-Based Incentive Payment System (MIPS), and the majority of MIPS-eligible clinicians still feel completely unprepared for success. With complicated and changing regulations, ensuring compliance can be a long and arduous process. Like most sizable goals, MIPS is best digested in small pieces, but it is hard to tell where to start sometimes. That is why we are going give you an order of operations to follow to ensure MIPS survival.
Topics: PRO Tips, MACRA & MIPS, CMS, Eligibility
One of the trickiest aspects of the new CMS Quality Payment Program is understanding how to report MIPS as a group. MIPS group reporting is when a TIN of 2 or more providers decides to report their MIPS measures and activities on the group (TIN) level, rather than on the individual (TIN+NPI) level. This could be an advantage to a practice that has a few providers who struggle to find measures that are relevant to them personally, or a practice exercising the "test option" of MIPS reporting for 2017. Eligible Clinicians must report either individually or as a group consistently across all MIPS performance categories.
Topics: MACRA & MIPS, Policy, Eligibility
Top Three Questions about Advanced Alternative Payment Model (APM) Participation
On October 14, 2016, the Department of Health and Human Services release the MACRA Quality Payment Program Final Rule. According to the Executive Summary of the Final Rule, the aims of the Quality Payment Program are to : "(1) support care improvement by focusing on better outcomes for patients, decreased provider burden, and preservation of independent clinical practice; (2) promote adoption of Alternative Payment Models that align incentives across healthcare stakeholders; and (3) advance existing efforts of Delivery System Reform, including ensuring a smooth transition to a new system that promotes high-quality, efficient care through unification of CMS legacy programs."[1]
Topics: MACRA & MIPS, Policy, Eligibility, APMs