Today, the Department of Health and Human Services (HHS) released the final rule with comment period for the Quality Payment Program under MACRA. Consistent with what was discussed in the proposed rule, the MACRA Quality Payment Program will have two tracks: (1) Advanced Alternative Payment Models (APMs) and the Merit-Based Incentive Payment System (MIPS).
The final rule differs from the proposed rule in ways that reflect stakeholder feedback from the proposed rule comment period. Specifically, it addresses improving support for small and independent practices, expanding opportunities to participate in Advanced APMs, implementing transition options, and connecting statutory domains into one unified program that supports clinician-driven quality improvement. In this summary, we will be focusing on the changes and details relevant to the Merit-Based Incentive Payment System (MIPS), but look for a future summary of Advanced Alternative Payment Models (APMs)!
In this summary:
Eligibility Updates
The specifications for MIPS eligible clinicians has not been updated since the proposed rule, with the exception of the adjustment of the low-volume threshold.
MIPS Low-Volume Threshold
The low-volume threshold has been made easier to meet from the initial proposed threshold. Now, to be considered low volume, a provider must bill less than or equal to $30,000 OR see less than 100 Medicare Part B beneficiaries.
From the Executive Summary of the final rule:
"For 2017, many small practices will be excluded from new requirements due to the low-volume threshold, which has been set at less than or equal to $30,000 in Medicare Part B allowed charges or less than or equal to 100 Medicare patients, representing 32.5 percent of pre-exclusion Medicare clinicians but only 5 percent of Medicare Part B spending." [1]
Performance Category Updates
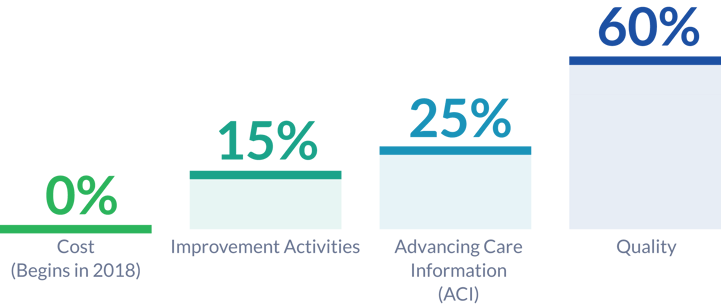
One of the biggest changes presented by the final rule is the reweighting of the MIPS performance categories. Quality is now worth 60% of the MIPS Composite Performance Score (MIPS CPS), and the Cost Performance Category (previously called Resource Use) is now going to be weighted for 0 for the 2017 performance period.
 Quality Performance Category
Quality Performance Category
To fully participate in the quality performance category, eligible clinicians or groups will report 6 measures including an outcome measure if possible. If there are no applicable outcome measures, then a participant must report a high-priority measure. If fewer than six measures can be reported, then participants should report all applicable measures. These measures must be reported for a minimum of a 90-day performance period.
As we've mentioned in previous posts, the quality performance category is closely related to the Physician Quality Reporting System (PQRS) which is to be sunsetted in 2017. One of the major changes between these two programs is the dissolution of the measure group reporting option. Instead, MIPS-eligible clinicians are able to report "specialty-specific measure sets." If six or more measures exist in a set, then a participant only has to report 6 measures (including one outcome measure, or a high priority measure if no outcome measure is applicable). If a measure set has less than 6 measures, then participants are expected to report the whole set.
![]()
Advancing Care Information Performance Category
In the proposed rule, it was suggested that eligible groups and clinicians report to 11 advancing care information (ACI) measures (from 6 objectives). The final rule has revised this suggestion, reducing the number of required measures to five. Participants can still report as many measures as they would like from this category, and will recieve bonus points to the ACI category score for doing so.
Additionally, for 2017, eligible clinicians and groups can recieve bonus points to their ACI category score for completeing an activity from the improvement activities performance category that utilizes certified electronic health record technology (CEHRT). The ACI performance category is still worth 25% of your MIPS CPS.
 Improvement Activities Peformance Category
Improvement Activities Peformance Category
The clinical practice improvement activities performance category from the proposed rule has been shorted to improvement activities. It will still be worth 15% of your MIPS Composite Performance Score (MIPS CPS), however, the number of required activities has been reduced. Now, participants must either report two high-weight improvement activities, or four medium-weight improvement activities. Eligible clinicians and groups from small practices, rural practices, or practices located in geographic health professional shortage areas (HPSAs), and non-patient facing MIPS-eligible clinicians will only have to report one high-weight improvement activity or two medium-weight activities.
As mentioned above, activities that utilize CEHRT will not only count for the improvement activities performance category score, but the ACI performance category score as well.
![]()
Cost Performance Category
The resource use performance category of the proposed rule has been renamed the cost performance category in accordance to comments recieved during the proposed rule feedback period. Additionally, and more significantly, it has been weighted to 0% of the MIPS CPS for the performance year of 2017. The plan as of now is to gradually increase it to 30% of the MIPS CPS by the payment year of 2021 (performance year of 2019).
This is part one of a two part summary of the final rule release. In part two, we will cover the MIPS pacing options, which should greatly reduce the burden of quality reporting!
Citations
[1] The Department of Health and Human Services. (2016, Oct. 14). Executive Summary; Medicare Program; Merit-based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Incentive under the Physician Fee Schedule, and Criteria for Physician-Focused Payment Models. Retrieved from https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf
[2] Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Final Rule, 42 CFR § 414 (2016). [CMS-5517-FC]
[3] Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Proposed Rule, 42 CFR § 414 (2016).



