Today, the Department of Health and Human Services (HHS) released the final rule with comment period for the Quality Payment Program under MACRA. Consistent with what was discussed in the proposed rule, the MACRA Quality Payment Program will have two tracks: (1) Advanced Alternative Payment Models (APMs) and the Merit-Based Incentive Payment System (MIPS). This is part two of our summary of the final rule, and will cover the pacing options available under MIPS. To read more about MIPS Eligibility and the MIPS performance categories, please check out Part 1!
In this summary:
Pacing Options Introduced
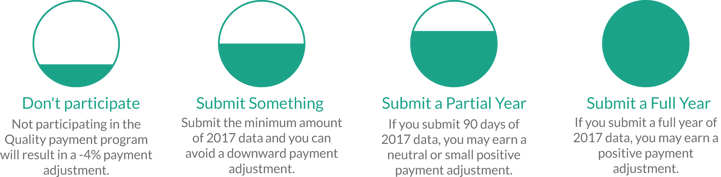
To ease the burden of transitioning to MACRA, CMS has introduced three pacing options for at least the performance year of 2017. Regarding the inclusion of these options for additional performance periods, the Executive Summary of the final rule states:
"We anticipate that the iterative learning and development period will last longer than the first year, CY 2017, of the program as we move towards a steady state; therefore, we envision CY 2018 to also be transitional in nature to provide a ramp-up of the program and of the performance thresholds." [1]
Each pacing option has different reporting specifications, however, all three options offer the safety of knowing the MIPS negative payment adjustment can be avoided. The final rule states the performance threshold for MIPS will be three (3) points, and so long as this is successfully met, no penalty will be attributed to your 2019 billing.
 Report Fully (70-100 points)
Report Fully (70-100 points)
Eligible clinicians who completely report to all three weighted performance categories will be eligible for a moderate positive payment adjustment. To review, complete reporting would be reporting 6 measures for the Quality Component, acheiving 40 points (2 high-weight activities, 4 medium-weight activities, or a mix) for the Improvement Activities Category, and completing 5 measures in the ACI Category for the full 2017 performance period (January 1, 2017 through December 31, 2017).
![]()
Submit Partially (4-69 points)
Eligible Clinicians who submit "more than minimal" data for the three weighted MIPS Performance Categories for at least 90 days will be eligible for a slight positive payment adjustment. Longer reporting periods will be more likely to result in higher incentives, as will reporting as to the full requirements of each performance category.
 Submit minimally (3 points)
Submit minimally (3 points)
Minimal reporting for MIPS is considered to be either:
- one measure from the Quality Performance Category
- one activity from the Improvement Activities Category
-OR- - five measures from the Advancing Care Information (ACI) Category
Successfully fulfilling any one of those three options will result in the avoidance of the 4% negative payment adjustment, but will not result in any positive payment adjustment. Additionally, failing to meet this baseline will result in a negative payment adjustment.
In conclusion, there is a lot to consider now that the final rule has been released. Here at the Healthmonix Advisor, we are going to continue to digest this new, 2,398 (!) page guide, and will be publishing summaries and insights to help you prepare for the upcoming transition.
Citations
[1] The Department of Health and Human Services. (2016, Oct. 14). Executive Summary; Medicare Program; Merit-based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Incentive under the Physician Fee Schedule, and Criteria for Physician-Focused Payment Models. Retrieved from https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf
[2] Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Final Rule, 42 CFR § 414 (2016). [CMS-5517-FC]
[3] Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Proposed Rule, 42 CFR § 414 (2016).
