When reporting individual quality measures, 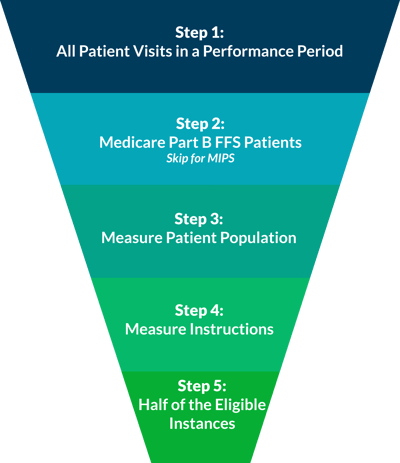 whether it be for PQRS this year, or for one of the performance categories of MIPS next year, you are expected to report at least 50% of your eligible instances for each measure. In our experience, this concept can be confusing when practically applied. Luckily, it can be disambigusted in five easy steps!
whether it be for PQRS this year, or for one of the performance categories of MIPS next year, you are expected to report at least 50% of your eligible instances for each measure. In our experience, this concept can be confusing when practically applied. Luckily, it can be disambigusted in five easy steps!
 Consider All Patient Visits for the Performance Period
Consider All Patient Visits for the Performance Period
A performance period for PQRS is based on a complete calendar year beginning on January 1 and ending on December 31.
For MIPS reporting, the performance period can range from a continuous 90-day period to the full calendar year.
 Narrow to Just Medicare Part B Beneficiaries (skip for MIPS)
Narrow to Just Medicare Part B Beneficiaries (skip for MIPS)
When reporting individual measures for PQRS, only report visits for Medicare Part B FFS Primary, Secondary, or Railroad. For MIPS reporting, all payers are considered eligible, so this step should be bypassed.
 Narrow by Patient Population
Narrow by Patient Population
Next, you will further refine your eligible patient visits by factors like age range, ICD-10 codes, and CPT codes, which can be found in the denominator section of individual measure descriptions.
 Follow the Measure Instructions
Follow the Measure Instructions
There is an instuction section within every individual measure description. In this section, you will see how frequently you must report each patient in the reporting period. After completing this step, you will be left with the eligible instances for the measure.
 Find 50% of Eligible Instances
Find 50% of Eligible Instances
To determine the minimum number of patient visits required, take the number from the previous step and divide it by 2. The resulting number will be the minimum number of included instances (50%) required for successful reporting. You may report 50%-100% of eligible instances.
For visual learners, we animated this process in a brief video:
If you would like further clarification, please feel free to schedule a meeting with one of our PQRS pros!


