If you are managing a Medicare Shared Savings Program accountable care organization (MSSP ACO), you have heard the mandate from the Centers for Medicare & Medicaid Services (CMS) to move to eCQM/CQM reporting, replacing the Web Interface reporting. You may also be aware of the significant pushback that ACOs, collectively and independently, have provided to CMS. At this year’s fall National Association of ACOs (NAACOS) conference, the tenor changed to accepting the move, optional in 2022 through 2024, but required in 2025.

Energy is now focused on acceleration of technical readiness, attempting to reduce the administrative burden, and avoidance of unintended consequences. NAACOS polled its members, which represent a significant percentage of MSSP participants, and found that 62% of respondents said they will not be ready, or are unsure as to their ability, to report eCQMs/ CQMs through the APM Performance Pathway (APP) requirements by 2025.
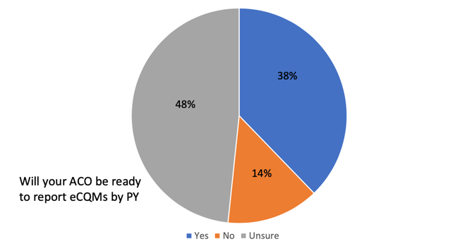
*Source: 2022 Fall NAACOS conference, The Transition to eCQMs: Multistakeholder Round Table Discussion
Other interesting finding from NAACOS's research:
- 10% of respondents plan to report eCQMs/CQMs in 2022, 13% in 2023 and 18% in 2024 while 40% are unsure when they will report eCQMs
- Costs, workflow redesigns ranked as top concerns
- 57% of ACO respondents anticipate needing the support of a third-party data aggregator (who is not the EHR vendor)
- Only 17% of respondents have one EMR (meaning the rest of the ACOs will need to aggregate data to achieve the necessary eCQM/CQM reporting)
Key issues in moving to successful eCQM/CQM tracking and reporting were identified as follows:
- Data Standards and Interoperability: The current state of data standards and interoperability make it difficult for ACOs to meet the reporting requirements successfully.
- All Payer Data: The shift to all payer data has unintended consequences and will result in ACOs being measured not solely on clinical quality of care provided, but rather the composition of the ACO and the payer mix.
- Patient Matching: There is a general lack of experience and solutions readily available to address patient matching needs. If ACOs are working to combine data, how accurate does their patient matching algorithm need to be, and where can reliable solutions be found.
- Workflow Changes: Work being done by EHRs and vendors may eventually reduce administrative burdens associated with reporting, however they still may require significant workflow changes to capture appropriate information in the EHR in the appropriate location. These burdens and costs must be accounted for when developing timelines for changing measure sets and specifications.
- Costs & Admin Burdens: ACOs face significant costs and administrative burdens to implement changes necessary to report eCQMs/CQMs and are not being provided with any additional funding to make such changes.
- Data Validity: ACOs must ensure that the data used for quality measurement are valid and representative of ACO performance using a broader patient population (data completeness requirements). The requirements as outlined in MIPS should be revaluated for ACOs, as there are different challenges ACOs face when reporting eCQMs/CQMs.
What does this mean to an ACO? It appears that while CMS may continue to refine the requirements, it is clear that the obligation to report is here to stay. ACOs must work to construct and execute a plan to enable successful reporting by 2025, and that means starting now.
Healthmonix's APP Impact enables ACOs to optimize eCQM/CQM scores by 23% and continue to see shared savings. Contact us to learn about our integrated approach.

