With the release of the 2020 feedback report detailing the 2.2% maximum possible payment adjustment and the release of the 2022 Proposed Rule, MIPS participants find themselves wrestling with lingering disappointment from participation in the program in previous years, and resistance to the idea that MIPS will be financially rewarding and challenging, in terms of reporting requirements, in 2021 and beyond.
This is the second in a series of blog posts on the 2020 payment adjustment and the 2022 Proposed Rule, that will address this sense of disappointment and show how the future of MIPS will contain much more rigorous program requirements and create greater financial rewards. To see financial and program success, you will need to be prepared to meet the new challenges. We have the guidance you need to succeed in 2021 and beyond.
Read More
Topics:
MACRA & MIPS,
Quality Performance Category,
Cost Performance Category,
2022 PFS Proposed Rule
With the release of the 2020 feedback report detailing the 2.2% maximum possible payment adjustment and the release of the 2022 Proposed Rule, MIPS participants find themselves wrestling with lingering disappointment from participation in the program in previous years, and resistance to the idea that MIPS will be financially rewarding and challenging, in terms of reporting requirements, in 2021 and beyond.
Read More
Topics:
MACRA & MIPS,
COVID-19,
2022 PFS Proposed Rule
As we move into 2021 and beyond, we see CMS putting some real teeth into the Merit-based Incentive Payment System (MIPS) program. This is the first year where we see more than two percent incentives possible. Exemptions and exclusions are narrowing. Participants in other value-based programs are being forced into MIPS reporting because of higher thresholds for exclusion and elimination of other reporting options.
Read More
Topics:
MACRA & MIPS,
MIPS Value Pathways,
APM Performance Pathway
There has been much talk around MVPs in the CMS quality reporting arena. MVP means MIPS Value Pathway, and it’s a reporting framework that CMS is communicating as (a) the next evolution of MIPS and (b) a transition tool for getting to other alternative payment modules. As CMS continues to define and refine their vision of the MVPs, they have started to call the current framework 'traditional MIPS' to prepare for the inclusion of the MVP option. You’ll see this when you visit the QPP site. That said, how can MVPs affect MIPS?
Read More
Topics:
MACRA & MIPS,
CMS,
2021 PFS Proposed Rule,
MIPS Value Pathways
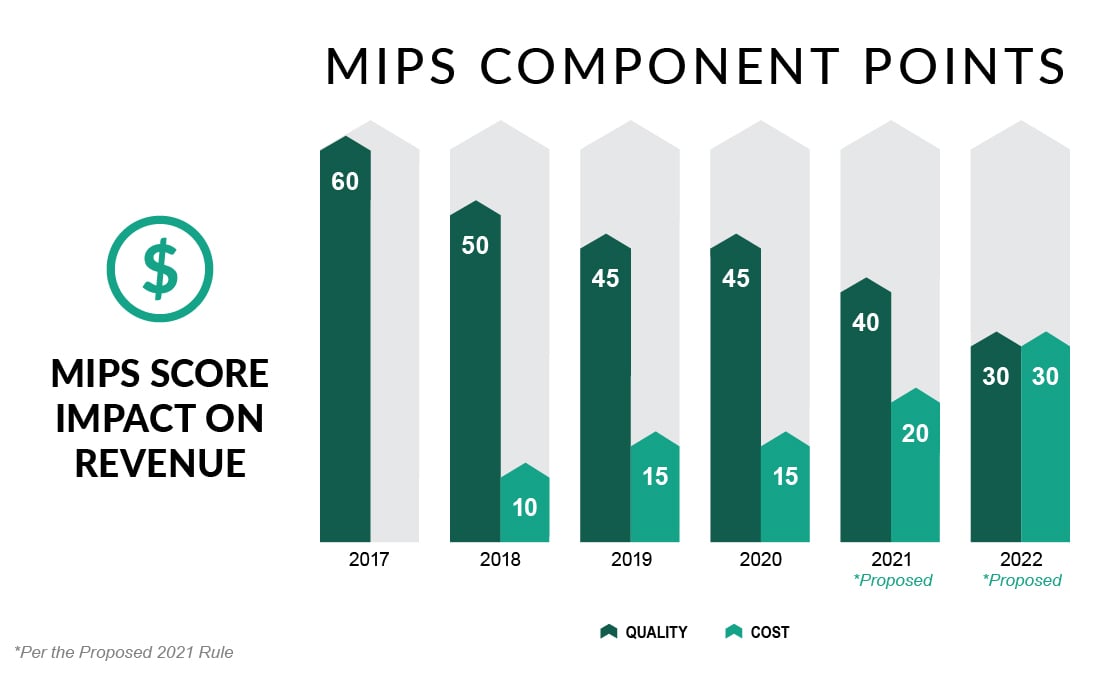
For years, we’ve heard that the Merit-based Incentive Payment System (MIPS) will provide a noticeable incentive for participants in this Medicare FFS program. And for years, there have been reasons why that has not occurred. First, CMS wanted to ‘start slow’ with the MIPS program in 2017 and 2018, so the caps on penalties and incentives were small. Then the potential penalties and incentives were raised, but the threshold for qualifying for an incentive remained low. This, coupled with the program’s budget neutrality meant there was not much revenue to distribute to high performers. Then COVID-19 negated much of the program for the last two years. So here we are, in year five, and we see that the program, for the first time, will have a significant downside and upside potential.
Read More
Topics:
MACRA & MIPS,
CMS,
APMs,
Cost Performance Category,
2021 PFS Final Rule
The long-awaited CY 2021 Medicare Physician Fee Schedule Final Rule update is now here. Despite the disruptions of the Public Health Emergency COVID-19, participation in performance year 2019 was strong. Thus the 2021 Final Rule moved forward with finalizing a number of proposed changes, including a higher performance threshold for performance year 2021, anticipated changes in weight to the Quality and Cost performance categories of the Merit-based Incentive Payment System (MIPS), and the introduction of the APM Performance Pathway. Other expected initiatives, such as MIPS Value Pathways, the requirement for registries to build their own benchmarks for certain measures, and the sunsetting of the CMS Web Interface, have been pushed back to at least the 2022 performance year.
Read More
Topics:
MACRA & MIPS,
APMs,
COVID-19,
2021 PFS Proposed Rule,
APM Performance Pathway
Clinicians participating in the Merit-Based Incentive Payment System (MIPS) are set to finally receive a worthwhile financial return for 2021 reporting. Providers have been unsure whether incentive returns of less than 2% justifies shifting focus to achieve a high score in the program. A provider collecting $400,000 in Medicare Part B payments in 2020 will only receive $6,700 for scoring well in 2018 quality payment program (QPP) performance. While this does produce a positive return on investment, it may cause practices to question whether it is worth the effort required to track and report measures.
Read More
Topics:
MACRA & MIPS,
Policy
The last 90 days of the year. Many might be ready to say goodbye to 2020 as a year filled with challenges, adjustments and ever-shifting expectations in our personal and professional lives. For those clinicians who are eligible for participation in the Merit-Based Incentive Payment System (MIPS), the last 90 days of the year also represents the beginning of some measurement periods and the final opportunity to improve in others.
Read More
Topics:
PRO Tips,
MACRA & MIPS,
Quality Performance Category,
IA Performance Category,
Cost Performance Category,
PI Performance Category
The 2021 Proposed Rule was released last week, and there are some potential changes that you should keep your eye on. Scouring through the entire release, it’s apparent that the Centers for Medicare & Medicaid Services (CMS) kept to their two main objectives:
- Minimize changes to reduce the burden on providers digging out of COVID-19
- Keep the momentum of the Quality Payment program moving forward
Read More
Topics:
MACRA & MIPS,
CMS,
Policy,
2021 PFS Proposed Rule
The quick answer is NO!
There has been quite a bit of discussion, and some press, about the reporting period for MIPS for 2020. I have seen a few articles saying that no data reflecting services provided January 1, 2020 through June 30, 2020 will be used in the Center for Medicare & Medicaid Services (CMS’s) calculations for the Medicare quality reporting and value-based purchasing programs. However, if you read the Quality Payment Program – COVID-19 Response, Updated 6/24/2020, there is no mention of an all-inclusive change to the reporting period.
Read More
Topics:
MACRA & MIPS,
CMS,
Industry insights