With 2022 MIPS final scores available, hospitals and health systems have seen the Cost category produce a major impact on their overall MIPS scores.
Before CMS added the Cost category to 2022 MIPS scores, hospitals had little insight into how it would impact MIPS scores. With scores out, we see that many hospitals and health systems were scored on over 10 Cost category measures. That’s a large amount of data to sift through and analyze.
-4.png?width=1200&name=Untitled%20design%20(1)-4.png)
Hospitals have paid attention to the MSPB measure for years. MIPS features a similar measure, the Medicare Spending Per Beneficiary-Clinician (MSPB-C) measure.
For medical MS-DRGs(Medicare Severity Diagnosis Related Groups), CMS attributes the measure episode to a clinician group that provides at least 30 percent of the evaluation and management (E&M) services on Medicare Part B Physician/Supplier claims during the inpatient stay (including admission and discharge days). For episodes in which the index admission has a surgical MS-DRG, the episode is attributed to the TIN that performed the related surgical procedure during the inpatient stay.
For the measure, CMS reviews and includes all inpatient stays across the country for Medicare patients. The calculation includes the total cost from 3 days before admission until 30 days post-discharge. CMS does exclude services identified as unlikely to be influenced by the clinician’s care decisions. All costs related to the stay, including inpatient, outpatient, professional, laboratory, and post-acute care, are included.
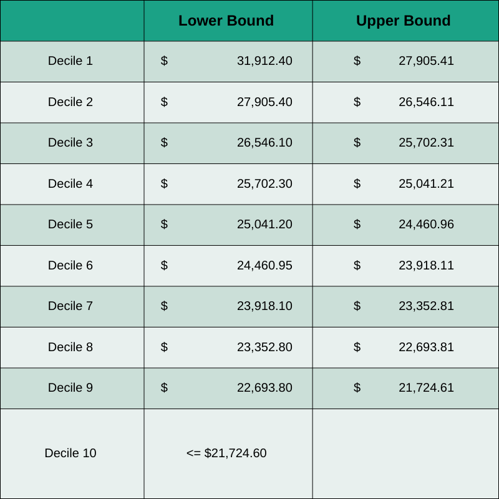
CMS calculates the average risk-adjusted costs for all episodes and stratifies into deciles for scoring purposes. Each decile represents 10 percent of the scores for that year across the measure. Each hospital TIN with at least 35 episodes will see a measure score of 1-10 points based on their relative calculation.
For 2022, CMS calculated the following deciles for the MSPB-C measure:
In addition to the MSPB-C measure, there are acute care measures (e.g. sepsis, COPD exacerbations) focused on inpatient stays and procedural measures (e.g. knee arthroplasty and elective outpatient PCI) focused on procedures where CMS sees large amounts of spending and costs that can perhaps be reduced. These measures are calculated and scored in a similar manner. Each measure varies a bit in terms of the relevant services included, the length of the post-discharge period included, and the risk-adjustment calculations.
Because measures are equally weighted (e.g. if MSPB-C has 300 episodes and Colon and Rectal resection has 13 episodes, they still have equal weight in the cost Category), some of the lesser performed procedures impact the Cost score as much as the more predominant procedures and inpatient stays. Hospitals can dive into each measure individually or perhaps look wholistically at the measures and the underlying costs.
To start, it might be worthwhile to dive into a measure that has fewer episodes. A smaller set of data could be easier to analyze. It could also make it easier to make changes that optimize care and cost.
Some important questions to consider for each of these measures are:
- How does your hospital compare with regional and national providers?
- Can you identify drivers of disparity in MSPB-C and other measure costs?
- Which MIPS cost measures show the highest variations?
- If your hospital is part of a system, how do system hospitals compare to each other?
- Where are the variations in cost arising?
- Can best practices be shared?
To better succeed in MIPS in the Cost category, hospital and health system leaders can begin by discussing these four points:
1. Understand the organization's capabilities to monitor the total cost of episodes of care.
What tools are in place to monitor episodes and the decisions being made in the care provided to patients? Providers need the ability to track the total cost of episodes and use the data to identify opportunities for intervention.
*For example, hospitals and health systems will want to use the data to identify unexpected variation in both price and utilization for further investigation. Variation can occur by provider, DRG, or other factors. The ability to review data and spot opportunities for improvement should be provided either internally or through an outside resource.
2. Recognize the need for claims data.Measuring and monitoring total cost of episodes requires access to claims data. Without claims data, it’s impossible to see the total cost for a patient across all care facilities.
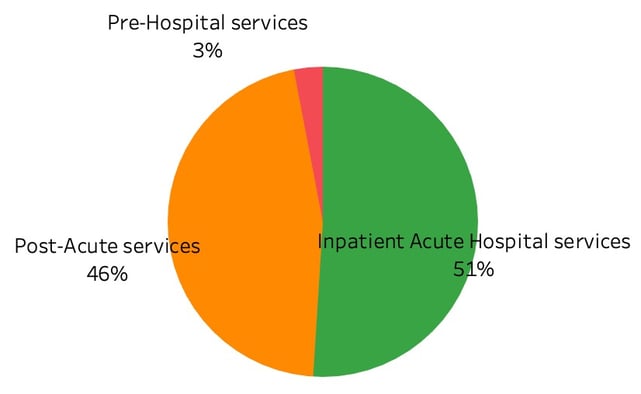
Looking at the MSPB-C and other episodes that are attributed to hospitals, the total cost for the episode is typically composed of costs where a large percent is outside the hospital’s domain. Claims can provide a full picture of the care during the entire episode duration.
Typical spend on MSPB-C episodes
For the post-acute period, the average costs break out as follows:
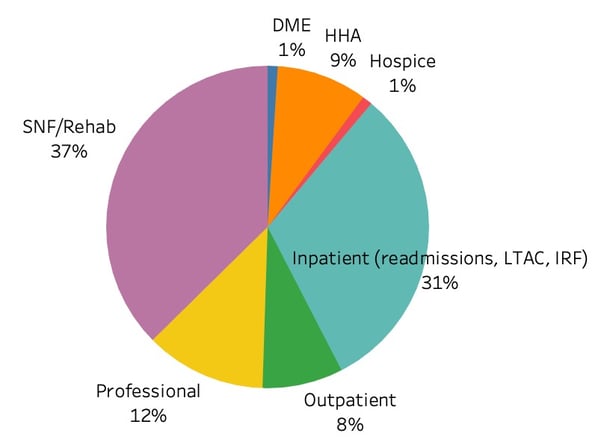
Identifying other major providers for patients across the care continuum is needed to provide more effective care models. A large percentage of Medicare patients receive post-acute services that can be a significant portion of the total cost. Professional services during the stay and after are also potentially variable and controllable.
Working with partners and building networks for collaborative care is helpful in optimizing care and costs.
4. Prepare for future iterations.MIPS cost measures will continue to evolve and reflect other care models, both from CMS and other payers. CMS is working to align measures with other value-based care programs.
Keeping an eye on the evolution of the measures and your performance can help in achieving more revenue and aligning with other payment models as they evolve.

