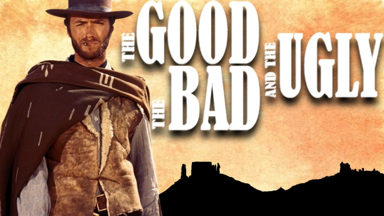
The 2020 final rule dropped yesterday and at first glance, there are some interesting highlights.
The good: CMS recognizes that the program is complex and confusing.
The bad: The remedies for this are still being developed
The ugly: We will need to be patient and change up what we do in years to come.
The good: Cost component weight is NOT increasing this year. In the proposed rule, Cost was to increase in its contribution proportion in the total score. However, due to the fact that providers have little insight into their scores, CMS is holding the component to 15% in 2020.
The bad: The performance threshold is rising to 45 points (from 30 in 2019). This makes it more challenging to receive an incentive. The exceptional performance threshold is rising to 85 points.
The ugly: Many quality measures that providers have reported for years either are removed or topped-out for 2020. Providers will need to take a hard look at the quality measures to report going forward.
The good: There will be larger incentives in 2020 due to the higher thresholds and other changes to the system. Those that participate and do well will see more revenue from the program going forward
The bad: Those that don’t take the program seriously, or have ‘just passed’ in the past will have a tough time and may see penalties in future years.
The ugly: The final incentive revenues are a black box. Because of the way that the program operates, there is no definitive algorithm to compute ROI for the program.
The good: CMS is working to improve partnership with third parties, e.g. QCDRs and Registries. We hear stories over and over about the issues with some of thes ‘approved partners’ and hope that CMS continues to strengthen the requirements for participation.
The bad: There are still many organizations that oversell their services. We, at Healthmonix, believe that MIPS reporting is not a stand-alone ‘point’ service, but an output of a bigger effort to analyze population health, improve patient care and/or optimize revenue in the organization.
The ugly: Interoperability is still a struggle and little is being done to resolve this on a large scale. We work every day to better derive data out of EHRs, billing, and PM systems.
You can view CMS's summaries here: https://qpp.cms.gov/about/resource-library . Drop us a line and get us your perspective.

