For the first time since the COVID-19 Public Health Emergency (PHE), all eligible clinicians must engage with the MIPS program or face a stark 9% cut in Medicare Part B claim reimbursements. With the stakes raised this year, scores have become pivotal. Additionally, the threshold for avoiding penalties has jumped in recent years, making high scores a coveted achievement.
Within MIPS, the quality component demands each clinician or group to report on 6 quality measures. The scoring landscape, however, has shifted:
- Bonus points for eCQM and additional high-priority measures have been eliminated.
- The baseline score for measures has been reduced from 3 points to 0 for non-small practices, adding to the competitive tension.
Picking which 6 measures to report is more than a choice; it's a strategic decision that can significantly impact final scores. Here are key changes for 2024:
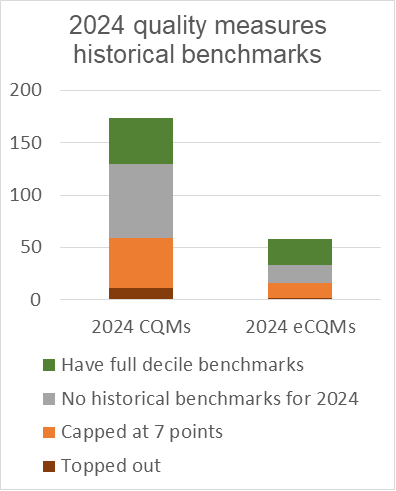
- Available measures sit at 173 CQMs and 58 eCQMs, a decrease from the 255 measures available in 2019.
- Fifty-nine CQMs and 16 eCQMs are topped out, demanding flawless reporting for a high score.
- Forty-eight CQMs and 14 eCQMs have a scoring cap of 7 points even with perfect performance.
- Two CQMs and 2 eCQMs are only available in MVPs.
- A significant number of measures — 71 CQMs and 17 eCQMs — don’t have historical benchmarks. The reasons for a lack of benchmarks include:
- Insufficient data from the 2022 performance year
- Measure suppression during the baseline period
- Issues with submitted data
- Changes in specifications that render them incomparable to previous periods
Quality measure benchmarks are the point of comparison used to score quality measures. Performance on each measure is assessed against its benchmark to determine how many points the measure earns. Measures that can be scored against a benchmark generally earn 1-10 points.
After considering these factors, we’re left with only 44 CQMs and 25 eCQMs that offer full decile scoring for 2024.
This is indeed a challenging climate for excelling in the quality category of MIPS. Clinicians and groups must navigate these intricacies with precision and foresight to ensure their reporting results in favorable outcomes.
How are benchmarks established?
CMS establishes benchmarks for each collection type: MIPS clinical quality measures (MIPS CQMs), electronic clinical quality measures (eCQMs), Qualified Clinical Data Registry (QCDR) measures, CMS web interface measures, the Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS survey measures, and Medicare Part B claims measures.
Whenever possible, historical data is used to establish benchmarks. Historical benchmarks for the 2024 performance period for eCQMs, MIPS CQMs, QCDR measures, and Medicare Part B claims measures are based on actual performance data submitted to the Quality Payment Program (QPP) for the 2022 performance period.
If there aren’t historical benchmarks for measures that have existed for at least 2 years, CMS may establish benchmarks at the end of the year after all data is submitted. CMS can establish performance period benchmarks when at least 20 instances of the measure are reported through the same collection type, meet data completeness and case-minimum requirements, and have a performance rate greater than 0% (or less than 100% for inverse measures). Performance period benchmarks will be established using data submitted by individual clinicians, groups, and virtual groups that are eligible for MIPS in the 2024 performance period.
Strategies for navigating MIPS quality measure selection and scoring in 2024
1. Explore new measures: With many standard measures from previous years retired or topped out, it's time to pivot. Analyze your practice's performance data early to identify newer or alternative measures that align with your clinical practices and areas of care.
2. Leverage a registry for insight: Using a registry can streamline measure tracking and let you evaluate a broader spectrum of measures. This approach can uncover underused measures where your practice may excel, potentially focusing on those with fewer patients, which might offer a more targeted approach.
3. Capitalize on measures with small denominators: Measures with smaller denominators can be advantageous, as they allow for more focused patient care and improvement efforts. This specificity can lead to higher performance scores as improvements can be implemented more rapidly and measured more directly.
4. Incorporate new measures into dashboards: Ensure that your registry dashboards include the new 2024 measures, particularly those with a base score of 7 points. Many of these new measures have broad applicability and can contribute to a robust scoring strategy.
5. Evaluate eCQM vs. CQM options: Benchmarks can vary between eCQMs and CQMs for the same measure. For instance, with Measure 1 (Diabetes: Hemoglobin A1c Poor Control >9%), the CQM option may yield higher scores for most performances. For performance levels under 15%, however, the eCQM version might provide a scoring advantage. It's prudent to assess both versions to maximize your score.
6. Consider an MVP: MVPs reduce the number of quality measures required to only 4. The benchmarks for those measures may also be difficult to achieve, so strategic consideration is needed.
7. Consider subgroups for MVPs: Dividing your group into multiple subgroups could optimize scores.Incorporating these strategies can provide a structured approach to quality measure selection and improve your MIPS score. Remember, it's essential to adapt to the changes each year brings and re-evaluate your strategy continuously. This helps you ensure compliance and maximize reimbursement potential.
Check out our webinar on the 2024 Quality measures. Register here.


