While many people on the East Coast were shifting into weekend mode Friday evening, CMS released the 2025 Medicare Physician Fee Schedule (PFS) Final Rule.
How will the 2025 PFS Final Rule affect our customers at Healthmonix? These are our initial impressions.
1. Stability is a priority
The last 4 years featured frequent changes to the MIPS program. The COVID-19 pandemic disrupted life for everyone, leading CMS to offer exemptions for MIPS reporting. Performance and data completeness thresholds changed year to year.
For 2025, CMS aims to bring stability to MIPS by carrying over current policies:
- The 75% data completeness threshold will continue through the 2028 performance year (We’ll see if this changes in upcoming rule-making).
- The 75-point performance threshold will hold for 2025.
With CMS keeping these thresholds, providers already know what targets they need to hit. That should reduce their burden and allow them to maintain their current workflows.
2. MIPS Value Pathways (MVPs) are the future — and maybe the present
2025 will mark the third year that MVPs are a reporting option in the MIPS program. CMS has expanded the number of available MVPs each year since their inception:
.png?width=400&name=White%20and%20Green%20Minimalist%20Table%20Comparison%20Chart%20(6).png)
The new MVPs are geared toward ophthalmology, dermatology, gastroenterology, pulmonology, urology, and surgical care. For providers like dermatologists, who have struggled to find enough relevant measures to their specialty in traditional MIPS, having an MVP should provide a better reporting choice, since the number of quality measures required to report is reduced to 4.
Around 80% of specialists will have an available MVP after the 2025 additions. That makes 2025 a great time for providers to consider reporting an MVP if they haven’t already.
Healthmonix has supported MVP reporting since it began. We’ll support all MVPs available in 2025 and the future. Best of all — Healthmonix customers can report traditional MIPS and MVPs side-by-side. If they report both, they’ll receive the higher score from CMS.
3. The changes to the Improvement Activities (IA) category are a plus
In past years, the IA category consisted of medium- and high-weighted measures. Providers needed to hit a point requirement based on the measures they selected to receive full credit in the category.
Starting with the 2025 performance year, CMS has decided that all IA measures should be considered high-priority. That means no more weighting for improvement activities.
The removal of IA measure weighting should lead to simplified scoring. It also aligns with CMS’ goal of refining and improving the inventory of IA measures.
Any CMS move toward simplified scoring is a plus for our customers.
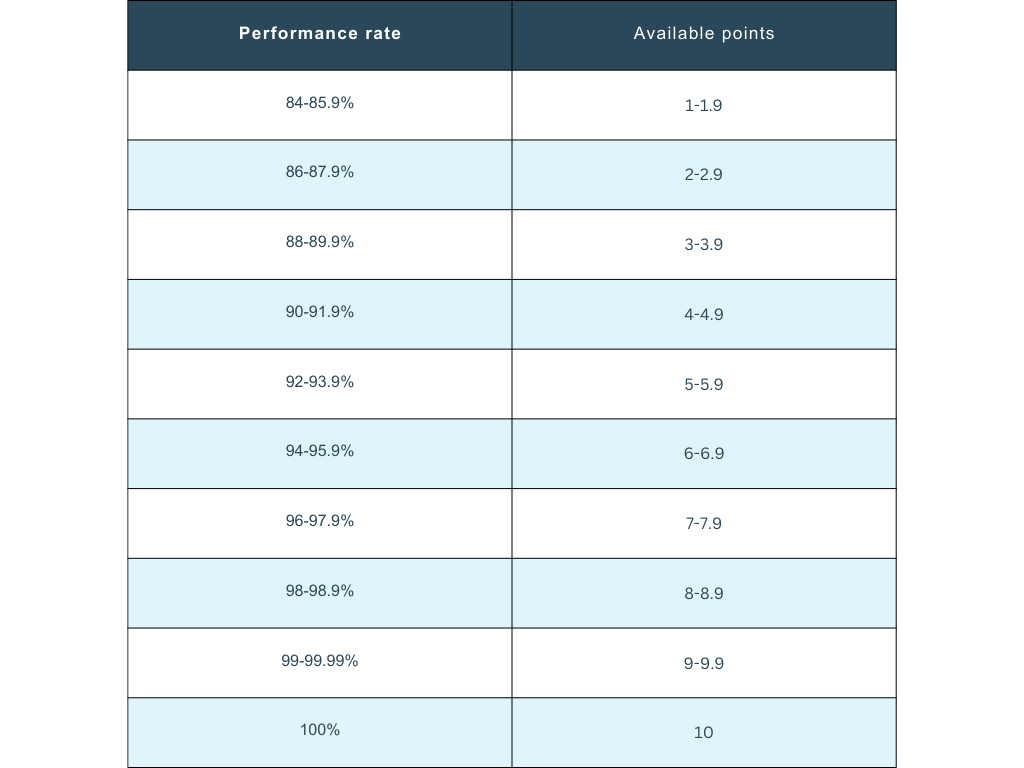
4. The shift in benchmarking for certain topped-out measures is a win
CMS recognized that topped-out measures in specialty sets with limited measure choice and lagging measure development have prevented some providers from meaningful MIPS participation. They’re addressing the issue by removing the 7-point cap for some topped-out measures in 2025.
The revised benchmarking for these measures is in the table below:
This screenshot reflects the measures that will have the new topped-out benchmarking applied in 2025:

Wrapping up
These initial impressions are just a starting point for how we see the 2025 PFS Final Rule affecting Healthmonix customers. We’ll share more information in the days and weeks ahead, including highlighting changes that will impact ACOs.
For more information on the 2025 PFS Final rule, check out our recent webinar. Two of our top MIPS experts, Healthmonix President Lauren Patrick and VP of Customer Success Michael Lewis, led an in-depth presentation of what the 2025 performance year will look like.

.png?width=1000&height=500&name=2025%20(1).png)