Over the last month, there’s been a lot of discussion around the 2020 Medicare Final Rule updates for the QPP and MIPS here at Healthmonix and with our partners and clients. While the last three years of the program were about getting healthcare providers up-to-speed with the program, now the focus is on challenging providers to adhere to tougher rules. High performers will reap significant rewards, others will see increasing downside.
Incentive / Penalty thresholds being raised
 Many providers have complained since the start of the program about its lack of teeth – everyone could ‘pass’ with minimal effort. This caused those that were really embracing the quality metrics and other aspects to fail to see a significant reward for all their efforts. That’s changing over the course of the next few years. The regulations state that the threshold for payment must be raised to an average performance by 2023. If we look at the prior years’ data, that would raise the incentive threshold to 74 points. CMS is on the path to that level by raisng the threshold to 45 in 2020 and 60 in 2021. By raising the thresholds for incentive, CMS is significantly raising the potential reward. For 2020, it’s projected at 6.25%, for 2021, significantly more.
Many providers have complained since the start of the program about its lack of teeth – everyone could ‘pass’ with minimal effort. This caused those that were really embracing the quality metrics and other aspects to fail to see a significant reward for all their efforts. That’s changing over the course of the next few years. The regulations state that the threshold for payment must be raised to an average performance by 2023. If we look at the prior years’ data, that would raise the incentive threshold to 74 points. CMS is on the path to that level by raisng the threshold to 45 in 2020 and 60 in 2021. By raising the thresholds for incentive, CMS is significantly raising the potential reward. For 2020, it’s projected at 6.25%, for 2021, significantly more.In addition, since the average performance was so high in past years, half of all providers were ‘exceptional performers’ – shades of Lake Wobegon. If you remember, there is a pool of $500 million that CMS shares between all exception performers. Since so many have achieved the 75 point threshold, CMS is raising that to 85 points to exclude about 180,000 from this pool.
On top of that – the criteria for success are getting tougher
With the performance thresholds being raised, the program curve is getting tougher. On top of that, each category of MIPS performance is seeing additional evolution in scoring.
Quality - Measures Reduced, Benchmarks Higher, Thresholds Higher
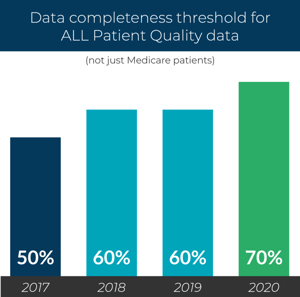 The data completeness threshold is being raised from 60 percent to 70 percent. This is not a challenge for most of our clients and partners, but does need to be considered. The average data completeness in years past (in the overall program) has been 75 percent, so some providers will need to step up their game.
The data completeness threshold is being raised from 60 percent to 70 percent. This is not a challenge for most of our clients and partners, but does need to be considered. The average data completeness in years past (in the overall program) has been 75 percent, so some providers will need to step up their game.
No cherry picking – do we hear this enough. At Healthmonix, we work to provide an accurate representation of data from providers, but apparently this is enough of an issue in the overall reporting that CMS keeps telling us this. Are you a cherry picker? I hope not…
Forty-two measures are gone this year (see our list here). The measures available for reporting are being culled to represent measures that are outcome-based, not duplicative, and have not been topped out. (The one easing is measures 1, A1c Not in Control, and 236, Controlling High Blood Pressure, which CMS have recognized as pushing providers too far in the treatment of their diabetic and hypertensive patients. )
Cost - More Measures cover additional participants, impact growing
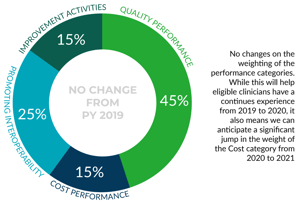
The cost component of MIPS has been updated to include 10 additional episode measures, as well as updating the MSPB measure so that now it’s called MSPB – Clinician and changing attribution and other factors in the TPCC measure. All this changes the providers that will be included in this category, as well as changing the benchmarks. Although Cost is not gaining additional weight in the MIPS Score for 2020, it still is mandated to be 30 percent of the score for 2022. Healthmonix is working to help shed light on these scores for providers, as now there is little insight into the scores that will be achieved, and no mechanism to determine how to improve. We feel strongly that scoring providers on measures where there is no understanding of the measure, nor any feedback prior to a final score is not serving anyone well. We’ll write more on this in upcoming blogs and white papers – sign up to be notified.
Improvement Activities - Groups must participate
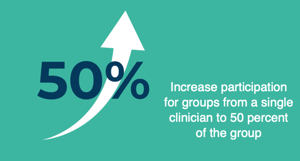
For group practices, only one provider needed to complete an Improvement Activity in years past in order to meet the criteria for completion. That is changing significantly for 2020. At least 50 percent of the providers need to participate AND they all need to participate during the same 90 day period. For large groups, this could take a pretty concerted effort. Actually many of the Activities are perhaps initiatives that organizations are already undertaking, so it may be awareness of the requirement and tracking more than a new initiative.
Several Activities have also been removed, changed or added, see our list here.
Medicare Value Pathways (MVP) coming in 2021 - Maybe?
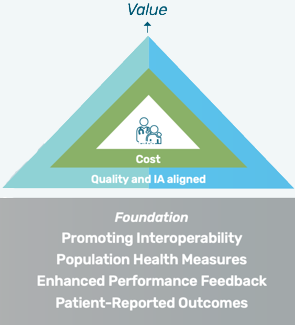 This year’s final rule discusses not only changes for the 2020 payment year, but also vision for the upcoming years. CMS has creates the framework for Medicare Value Pathways, which works to bring together the silos of the current MIPS program into a more focused model. This model advocates for:
This year’s final rule discusses not only changes for the 2020 payment year, but also vision for the upcoming years. CMS has creates the framework for Medicare Value Pathways, which works to bring together the silos of the current MIPS program into a more focused model. This model advocates for:· smaller sets of quality measures that are outcome-based
· improvement activities that align with the activities measures in the quality metrics
· cost measurement that also aligns with that focus.
This is a great concept. To date the program can feel disjointed and does not advocate for a comprehensive look toward value-based care. Details are still forthcoming and we question the implementation of this model--as we have seen in the past, defining a program that suits all providers is difficult, how do we define the metrics, how many MVPs will be needed for the program, and how will benchmarks be established.
Where do we go from here?
While MIPS has been a safer program than APMs, from the perspective of financial risk, it is becoming more challenging. Share your perspective on the changes in the comment section below. My next blog will focus on a few pathways to success in 2020.

