
The CY 2019 Medicare Physician Fee Schedule Final Rule involves a slew of regulatory changes that will apply to the 2019 performance year. Of course, wading through the final rule to find and understand the most important features of the policy can be grueling; but you’re in luck, because we’ve already done it so you don’t have to! In today’s blog, we’re focusing on the MIPS Improvement Activities (IA) category.
 Background
Background
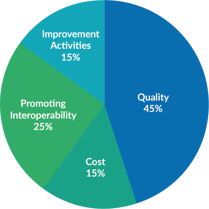
Performance in the Improvement Activities category will continue to account for 15% of the final MIPS score. Improvement Activities are defined as activities that would improve clinical practice or care delivery and, if effectively executed, are likely to result in improved outcomes. CMS will use the previously established data submission criteria, and exceptions for small, rural, geographical HPSA, and non-patient facing clinicians.
Weighting and Reporting Requirements
In previous years, “high” weight was based on the intensity of the activity. Now, however, CMS would instead prefer that “high” weight be assigned for an activity that directly addresses areas with the greatest impact on beneficiary care, safety, health, and well-being. Medium-weight activities remain worth 10 points, and high-weight activities worth 20 points.
The base requirements for the Improvement Activities performance category have changed very little. Full credit for this category will be awarded to participants who achieve 40 points (20 points for small or rural practices, HPSAs, non-patient facing clinicians, or APM participants).
Note: a clarification was made this year that a Patient Centered Medical Home must be attested to and will not “automatically” be classified by CMS as such. Previous wording was unclear on that issue.
Submission Criteria
CMS has established that, starting in Year 2 (2018), all data, including the attestation for Improvement Activities, must be submitted through either:
- Qualified registries;
- EHR submission mechanism;
- QCDR;
- CMS Web Interface;
- or attestation via the QPP portal.
The clinician must certify all activities were performed as stated, and the authorized Health IT Vendor, QCDR, or qualified registry would submit on their behalf.
Annual Call for Activities
In the CY 2018 QPP final rule, CMS formalized the Annual Call for Activities process for Year 3 and future years for adding possible new activities or providing modifications to the current activities in the IA. Stakeholders would apply one or more of the below criteria when submitting nominations for improvement activities:
- Relevance to an existing improvement activities subcategory (or a proposed new subcategory);
- Importance of an activity toward achieving improved beneficiary health outcome;
- Importance of an activity that could lead to improvement in practice to reduce health care disparities;
- Aligned with patient-centered medical homes;
- Focus on meaningful actions from the person and family's point of view;
- Support the patient's family or personal caregiver;
- Activities that may be considered for an advancing care information bonus;
- Representative of activities that multiple individual MIPS eligible clinicians or groups could perform (for example, primary care, specialty care);
- Feasible to implement, recognizing importance in minimizing burden, especially for small practices, practices in rural areas, or in areas designated as geographic HPSAs by HRSA;
- Evidence supports that an activity has a high probability of contributing to improved beneficiary health outcomes; or
- CMS is able to validate the activity.
CMS has also finalized the adoption of an additional criterion entitled “Include a public health emergency as determined by the Secretary” to the criteria for nominating new improvement activities beginning with the CY 2019 performance period and future years. CMS has also removed the following criterion: the bonus for promoting interoperability and thus the CEHRT bonus.
If you want to learn more, dig even deeper by enrolling in the free Value-Based Care Institute (VBCI) online course on Improvement Activities.

