Starting in January, 920 primary care practices will embark on the one of the newest payment models from the Centers for Medicare & Medicaid Services (CMS) via the Primary Care First (PCF) Program. The main criteria for participation in the program are:
- 70% or more of the practice’s collective billing must be for primary care services.
- Use of a 2015 Certified Electronic Health Record Technology (CEHRT) by the practice.
- At least 125 services provided for attributed Medicare beneficiaries.
Also, for the first year of the program, there is a limited geographical area for participation.

The Objectives of the Primary Care First (PCF) Program:
- Strengthening Doctor-Patient Relationship
- Enhancing Care for Patients with Complex Chronic Needs
- Focused Care for Seriously Ill Patients
- Minimized Administrative Burden
- Focused Financial Rewards on Improved Health Outcomes
There are two separate options for participation in the Primary Care First payment model:
- Primary Care First Payment Model
This option offers practices an opportunity to gain a 50% revenue boost with limited downside risk of 10%. Reducing cost of care, most notably by means of a reduction in hospital visits, will drive the desired outcomes for this program. Clinicians will also be expected to drive better patient care through engagement, access, and coordination all while increasing the clinician’s freedom to provide care that best suits their population.
- High Need Population and Seriously Ill Population (SIP) Option
This option is intended for those practices that will be addressing needs of the most vulnerable and sick patients. Patients will be identified for this program based on incidence of serious illness and a pattern of fragmented care. Payments will differ from the Primary Care First model and will reward practices based on stabilizing the patients’ health.
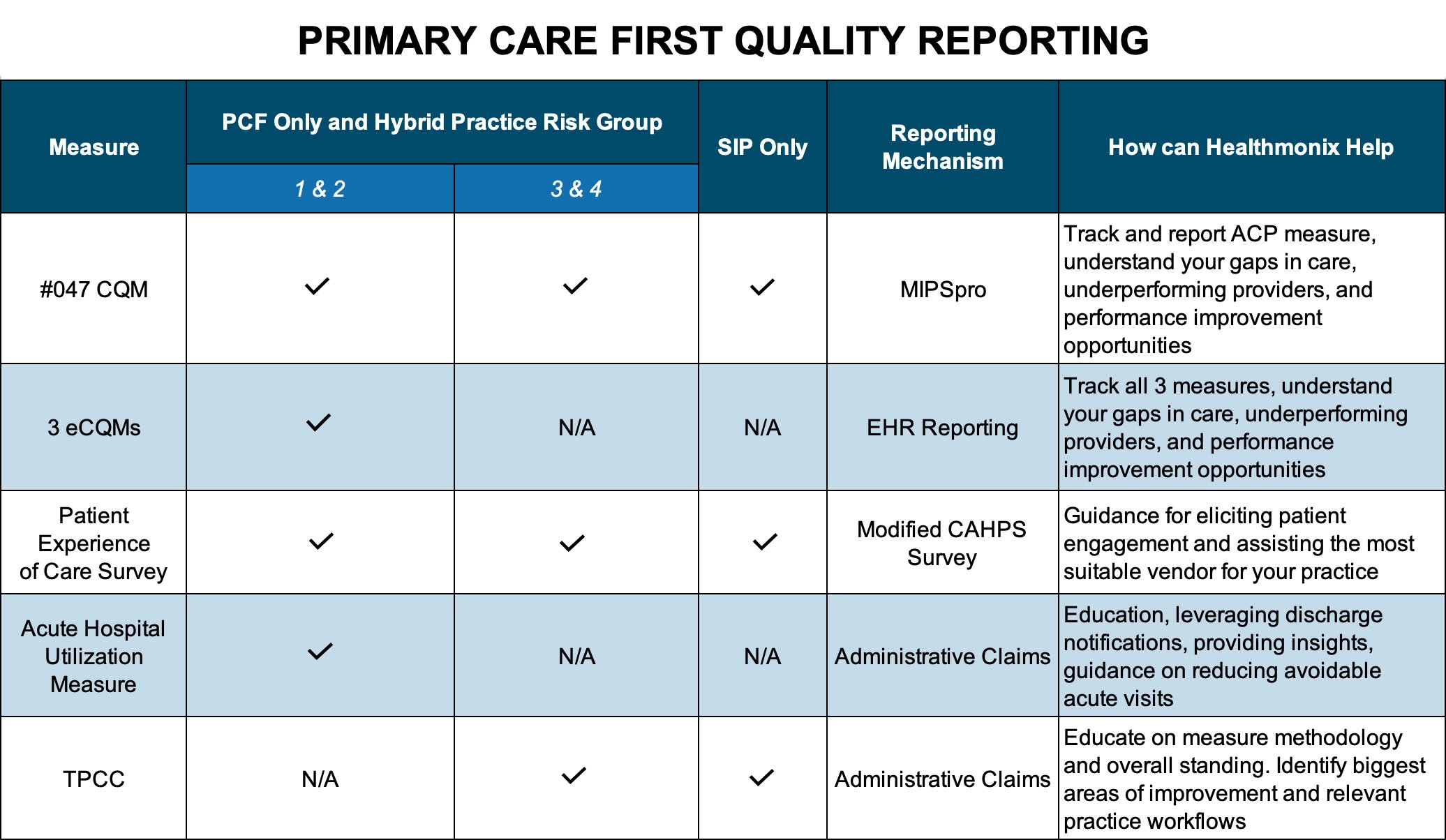
*A Hybrid model is also available for those that want to participate in both options.Like most payment models, Primary Care First practices will be required to report on quality metrics to CMS. The program is unique in that it will incorporate five independent quality measure types. Depending on their Risk Group Classifications, a practice may be required to participate in 3-4 of the below quality categories:
Other interesting features of this program that you should know:
- Private payers and Medicare Advantage programs have joined up with Medicare for this program around the country.
- Every physical location is considered a separate practice even if they share the same Tax ID Number (TIN).
- Practices must participate in a regional health information exchange (HIE) to be part of this program.
- Other value-based care payment options can overlap with the PCF program, such as Bundled Payments for Care Improvement Advanced (BCPI Advanced) and Oncology Care Model (OCM).
- Risk group classification are based off HCC scores for the practice’s entire patient population.
- There will be another application period for this program opening in early 2021, but only providers that are a current participant in the CPC+ program will be able to apply .
How can Healthmonix Help?
We are both a MIPS Qualified Registry (QR) and a Qualified Clinical Data Registry (QCDR) that easily tracks the required Advanced Care Plan measure. We’ve been a trusted source of this type of quality tracking and reporting for over a decade, and can integrate with your EHR to give you real-time access to your performance. Our PCF solution will help you maximize your score by allowing you to attack your gaps in care and identify your outlier clinicians.

