Quality scores matter!
The Medicare Shared Savings Program (MSSP) saved $1.8 billion for Medicare in 2022, according to last month’s announcement by the Centers for Medicare & Medicaid Services.1 This marks the second-highest yearly savings since the program’s start. It further underscores the program’s track record of consistently generating savings and delivering high-quality performance for the sixth consecutive year, as noted by CMS.

For an MSSP ACO to receive the maximum shared savings in 2022, they had to report quality measures and achieve a minimum Quality performance score. If the benchmark for the quality measures wasn’t met, the ACO didn’t receive its full financially earned savings.
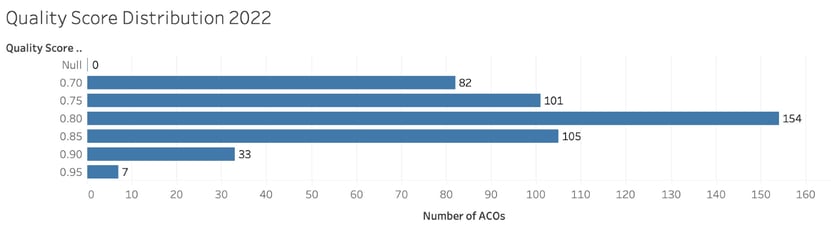
Here is the distribution of Quality scores achieved by ACOs in 2022:
Quality performance scoring
ACO Quality performance scores are based on applicable methodology for a performance year. In 2022, an ACO’s Quality performance score was calculated using the ACO’s performance on the quality measures reported under APP and any applicable quality improvement points. All MSSP ACOs were eligible to have the Shared Savings Program Quality EUC policy applied.
Under the Savings Program Quality EUC policy, if the ACO was able to report quality data via the APP and met the MIPS data completeness and case minimum requirements, the ACO’s Quality performance score was set to the higher of the ACO’s Quality performance score or the equivalent of the 30th percentile MIPS Quality Performance Category (QPC) score across all MIPS QPC scores, excluding entities/providers eligible for facility-based scoring. If the ACO was unable to report quality data and meet the MIPS data completeness and case minimum requirements, the ACO’s Quality performance score was set equal to the 30th percentile MIPS QPC score across all MIPS QPC scores, excluding entities/providers eligible for facility-based scoring.
Using that methodology, 39 of the 482 ACOs received the 30th percentile MIPS QPC score for 2022. The rest had scores ranging from 70.75-98.35.
With practices and EHR instances employing different unique patient identifiers (IDs), patient matching can be daunting. The absence of a universal primary key means we must rely on patient attributes such as name, date of birth, sex, and address to attempt the identification and matching of unique patients.
For 2022, no ACOs had a negative impact from Quality performance scoring. Great news! But what happens next?
We know that CMS is changing the methodology for Quality performance scoring for MSSP ACOs. The Web Interface is being sunset. CQM and eCQM — and perhaps Medicare CQM — reporting are becoming the required reporting approach.
We also know CMS has been somewhat forgiving in the last 3 years because of the COVID-19 Public Health Emergency, but that is being phased out. One big concern we all have is that the performance target isn’t known until after the performance year is complete. It’s been set at the 30th percentile in the past; CMS has indicated it’s moving to the 40th percentile in the future.
Here is the data for those benchmarks from 2018-2022:
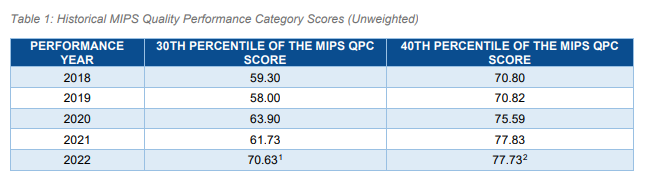
Some explanation:
- This data reflects the 30th percentile MIPS QPC score, consistent with the Performance Year (PY) 2022 MIPS performance feedback data provided by the Quality Payment Program during the MIPS Final Score Preview period
- This data reflects the 40th percentile MIPS QPC score, consistent with the PY 2022 MIPS performance feedback data provided by QPP during the MIPS Final Score Preview period 3.
Moving from Web Interface reporting to CQM and eCQM reporting
QPP has allowed large organizations, including ACOs, to use the CMS Web Interface reporting method to complete MIPS requirements since the program launched in 2017. This gave these organizations the choice to report a sampling of 248 patients (selected by Medicare Part B claims) across all their practices. CMS will completely sunset the CMS Web Interface reporting option by 2025.
Per current regulation, all MSSP ACOs must report either eCQMs or CQMs for all patients and all payers across all practices for 365 days of the year starting in 2025. There’s an alternative in the 2023 PFS Proposed Rule to allow Medicare CQMs, a new option that could lessen the burden going forward.
In the intervening years, options for quality reporting may be confusing and require planning by ACOs. ACOs may report both the CQM and eCQM, and the Web Interface options during the transition years. CMS will award the better of the scores from the 2 approaches until retiring the Web Interface. CMS is also offering alternatives for achieving a qualifying Quality score by reducing some target benchmarks and relaxing requirements during the transition.
What does the 2022 data tell us about CQM and eCQM reporting?
Here is a summary of the 2022 ACO quality measure scores:
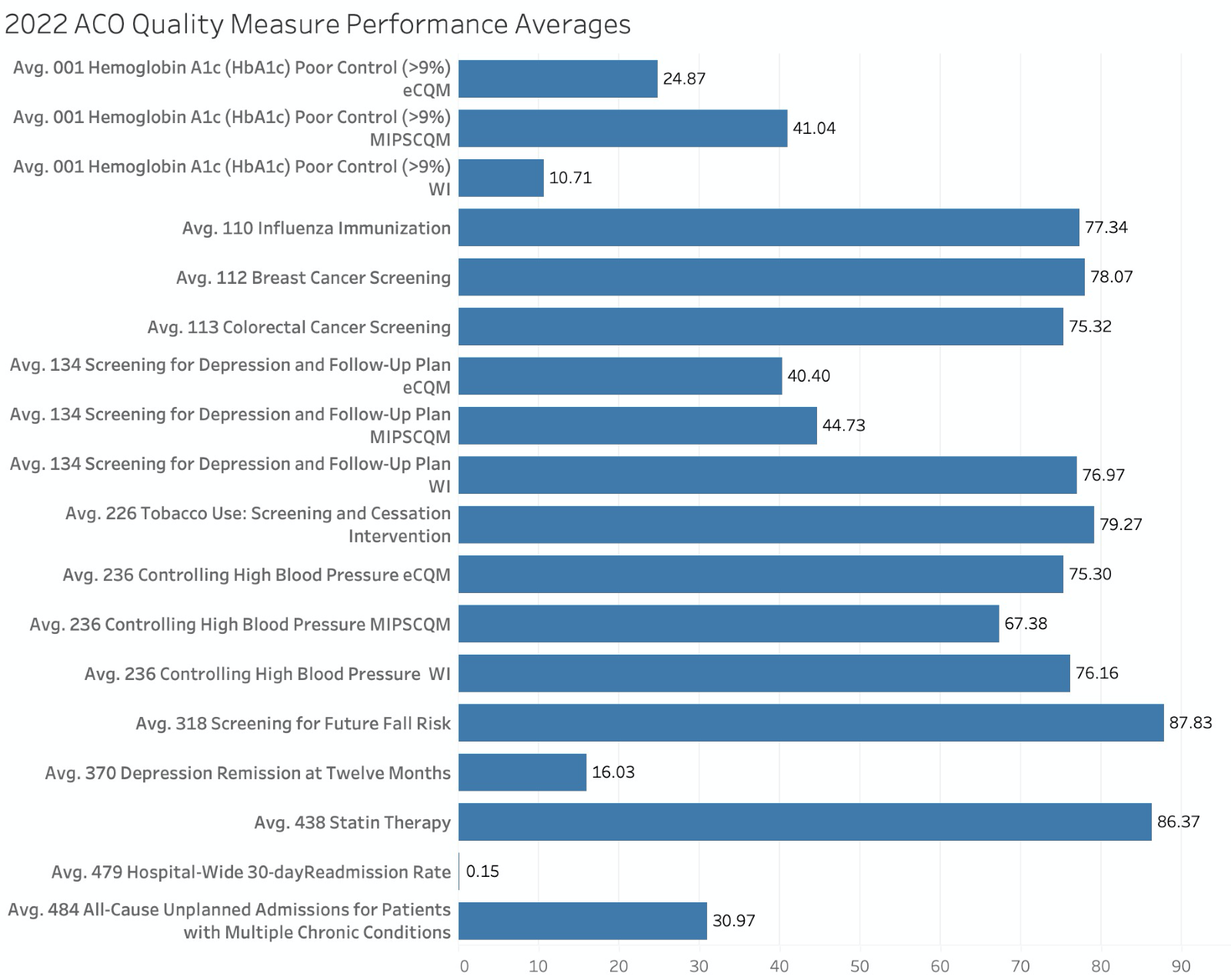
Here is a summary of the 2022 ACO quality measure scores:
It should be pointed out here that for the Web Interface and eCQM reporting, the ACO scores are better on average than the overall MIPS historical averages published by CMS. When we look at the MIPS CQM performance, however, ACO performance on the HbA1c Poor Control and Screening for Depression and Follow Up Plan was significantly lower than the MIPS historical averages. The performance on the Controlling High Blood Pressure CQM was similar. These MIPS CQMs are the measures many ACOs will use as we move into future performance years.
This once again underscores the need for ACOs to start thinking about CQM and eCQM reporting if they haven’t already done so. Consider these facts:
- ACOs need to achieve a 30th/40th percentile score that is retrospective.
- MIPS CQM performance for ACOs was lower than MIPS historical averages.
Therefore, a focus on strategies going forward is a must.
3.) https://www.cms.gov/files/document/medicare-shared-savings-program-performance-scores-equate-30th-and-40th-percentile-mips-quality.pdf
Click here to schedule an APP Impact demo/consultation

