Last week, CMS confirmed that 2022 MIPS scores for eligible providers will include the Cost performance category. Per CMS:
“For the 2020 and 2021 performance periods, CMS reweighted the MIPS Cost performance category to 0% as a result of the COVID-19 public health emergency (PHE). For the 2022 performance period/2024 MIPS payment year (hereafter written as “2022 performance period”), CMS conducted an empirical analysis to assess whether any or all cost measures were continually impacted by the COVID-19 PHE and, if so, whether it would be appropriate for CMS to reweight the Cost performance category again under § 414.1380(c)(2) or to exclude any individual cost measures.
Read on to learn more about how these changes may affect your MIPS participation and payment year.
.png?width=650&height=406&name=Untitled%20(Blog%20Graphic).png)
Cost measures analysis
“Our empirical analysis of the cost measures, and their underlying data, for the 2022 performance period showed that 24 of the 25 cost measures haven’t been significantly impacted by the COVID-19 PHE to the extent that it would be appropriate for CMS to reweight the Cost performance category again or to exclude any individual cost measures under our policy described in the section above. Generally, our analysis demonstrated that calculating the scores for these 24 cost measures would adequately capture and reflect the performance of MIPS-eligible clinicians. Our empirical analysis identified only the Simple Pneumonia with Hospitalization measure as warranting exclusion from our calculation of MIPS-eligible clinicians’ scores under the Cost performance category, as further discussed in Table 1 below.
Applying 30% to the Cost category
“On this basis, CMS has determined that it won’t automatically reweight the Cost performance category for all MIPS-eligible clinicians under our policies set forth in § 414.1380(c)(2) for the 2022 performance period. Unless an exception applies to an individual MIPS-eligible clinician or group under § 414.1380(b)(2) or § 414.1380(c)(2), CMS will apply the weight of 30% to the Cost performance category in CMS’s calculation of final scores under § 414.1380(c)(1)(ii) for the 2022 performance period.”
What does that mean?
Many MIPS-eligible providers will be surprised at their final score, as it’s likely to be lower than expected because of the Cost category score.
In the Cost category, providers can’t select the measures attributed to their MIPS score. The Cost category is scored retrospectively based on data providers probably haven’t seen. CMS reviews all claims for all Medicare patients and determines attribution based on data such as provider specialty, services performed, surgery code modifiers, and place of service.
Cost measures are scored based on total cost for the episode of care, not just the provider’s cost. The scores for each measure are based on the average episode cost for the attributed episodes compared to all others, and the score is scaled from 0-10 based on the comparisons.
So, to many, it appears a mystery box.
Many providers will receive Cost scores and find they average around 15 of 30 possible points. For most, this will bring their overall MIPS score down. If providers are losing 15 points off their total score because of Cost, their highest overall score is 85 even if they score perfectly in all other performance categories (Quality, Promoting Interoperability, and Improvement Activities).
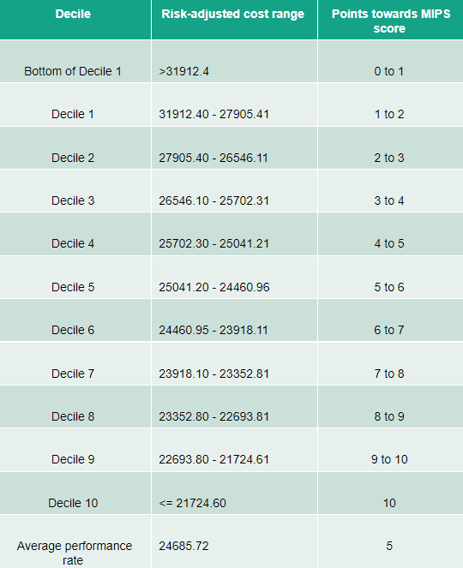
CMS has published the benchmarks for the cost measures for 2022 on the QPP website. They have included both the decile scores and the average for each cost measure (except Simple Pneumonia with Hospitalization).
This is MSPB-C, which is one of the most-applicable measures to providers:
For the MSPB-C measure, CMS will add up all services such as diagnostic tests, inpatient services, anesthesia, and aftercare attributes during the 3 days before and 30 days after the inpatient stay being attributed to the provider(s). For example:
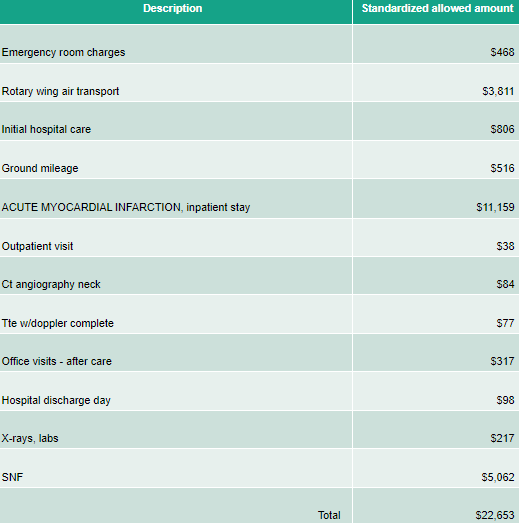
All of these services are summed up and included in the MSPB-C episode, which is then risk-adjusted. This episode is then attributed to a provider based on services provided. In this case, the entire episode would be attributed to the provider TIN rendering at least 30% of evaluation and management services during the inpatient admission.
If a provider’s episode average risk-adjusted cost was greater than $31,912, they would receive 0 out of 10 points for the MSPB-C measure. If the average episode cost was $25,041-$24,460, they would receive about 5 out of 10 points. And if the average cost was less than $21,724, they would receive 10 out of 10 points.
In summary, many providers will find it challenging to understand their final MIPS score for 2022. They will also find it more difficult to determine steps to continue doing well in the MIPS program in coming years.
Stay tuned for our next blog showing real-life examples of how the Cost category can impact your MIPS score.
CMS Notification: https://qpp-cm-prod-content.s3.amazonaws.com/uploads/2436/2022%20MIPS%20Cost%20Measure%20Exclusion%20Fact%20Sheet.pdf

