With the release of the 2023 PFS Final Rule, the Centers for Medicare & Medicaid Services (CMS) finalized most of the proposed changes for the QPP / Merit-based Incentive Payment System (MIPS) program that had been released in the Proposed Rule last July.
We are seeing that while the payment threshold is holding at 75 points, it can be tougher to achieve that threshold score with the changes in the program for 2023.
Some challenges:
- Quality measures that have historically had high scores will be topped out and/or removed from program. What does this mean? It will be harder to find Quality measures where you can achieve a full 10 points.
- CMS offers no tools to monitor the Cost performance category during the performance year. Providers are given scores based on their performance relative to other providers retrospectively. Scores will group around 15/30 points. What does this mean? More than likely, if any of the Cost category measures apply to your reporting, you will not achieve 15 of your 100 points in your MIPS score.
- MIPS Value Pathways (MVP) scoring is challenging. Each MVP includes at least one Cost measure. In addition, there is at least one population health measure applied to the score, and your team has no insight into what that score will be. What does this mean? Less insight into your final score if you are reporting an MVP.
- Because of the challenges of the various reporting options, "simple" reporting mechanisms, e.g. eCQMs from a certified electronic health record technology (CEHRT) may set up providers to actually see a penalty. What does this mean? If an average score from the Cost category is 15/30, and a provider / group achieves a perfect score for Promoting Interoperability (PI) and Improvement Activities (IA), a score of 20/30 in Quality, or an average of seven points per reported measure must be achieved. To do this, many providers will need to find specialty measures or work on performance improvement in their measures to meet the threshold to avoid a penalty. Often, an EHR / CEHRT reporting tool does not offer this opportunity to analyze and improve.
- There are many options for reporting. Each option will most likely result in a different score. What does this mean? We suggest beginning to collect your data early in the year and reviewing the results mid-year to determine the optimal path to reporting. From there, focus can put you on the path to the best outcome.
In 2023, MVPs offer an opportunity to focus on specialties and narrow the quality reporting requirement to only four measures. In addition, submission of an MVP restricts the Cost measures that are applied to only the Cost measure that is applicable to that MVP.
Utilizing our registry is a great way to analyze your data and determine the most advantageous reporting strategy. The registry that Healthmonix provides allows for determination of scores for eCQMs, CQMs, MVPs, APMs, individuals, and groups.
How do MVPs work and what are the challenges?
MVPs are a subset of previously defined measures and activities that were used under traditional MIPS, but they have been grouped for a specific disease or specialty. According to CMS, "the goal is to move away from siloed reporting of measures and activities towards focused sets of measures and activities that are more meaningful to a clinician's practice, specialty, or public health priority."
Accordingly, the MVP framework will "align and connect measures and activities across the Quality, Cost, and Improvement Activities performance categories." The MVPs include the Promoting Interoperability performance category and population health claims-based measures as foundational elements.
The measures and activities that will be reported under MVPs will consist of limited, connected, complementary measures and activities that are defined for that particular pathway. Thus, practices using the MVP framework will no longer be able to report on individual measures of their own choosing.
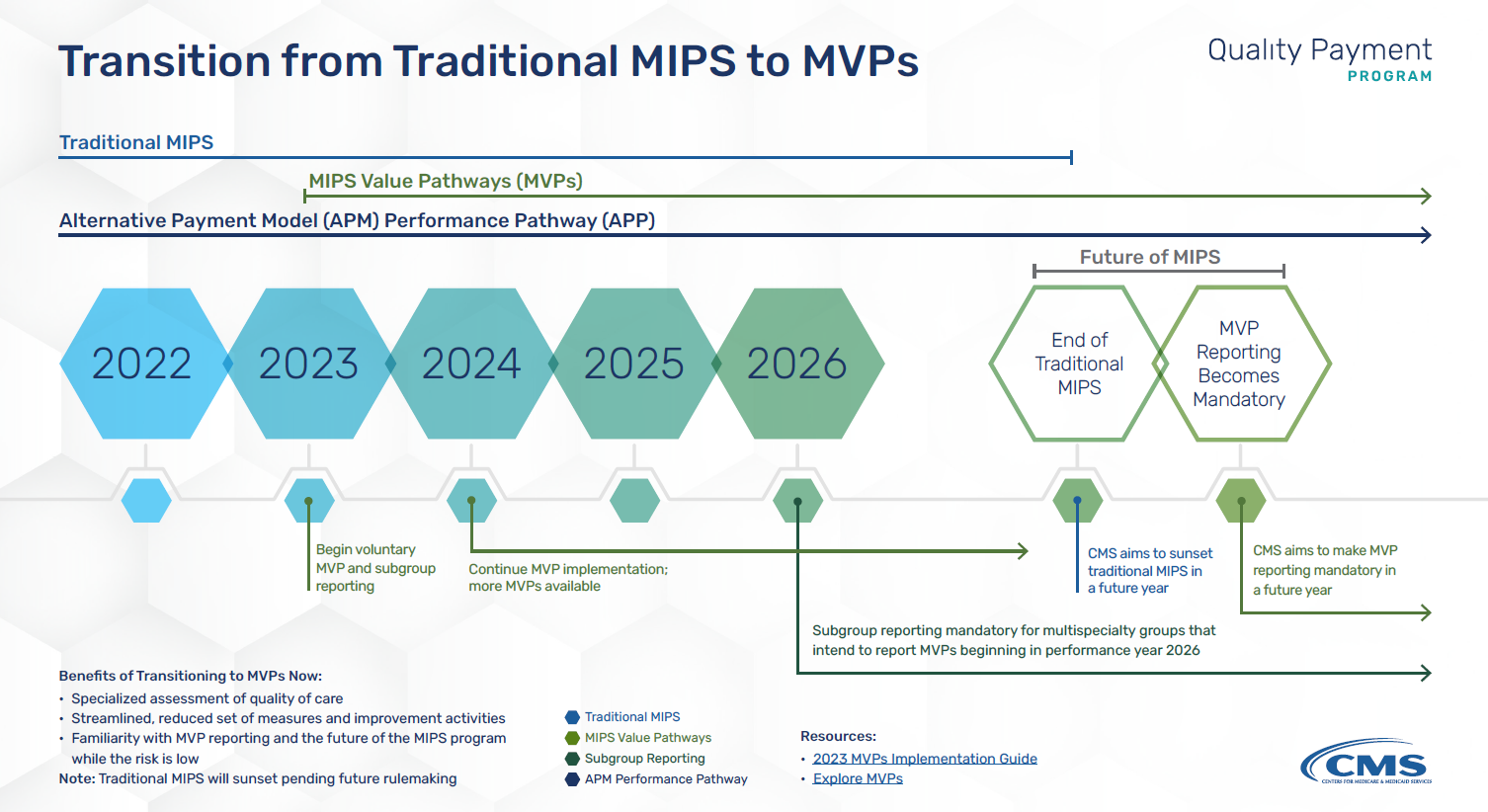
*graphic from qpp.coms.gov Resource Library
What are the participation options?
For the 2023-2025 performance years, a participant is defined as follows:
- An individual clinician
- A single- or multispecialty group
- A subgroup
- An alternative payment model (APM) entity
An MVP participant can only participate in a single MVP for each reporting period. However, an individual clinician can participate in multiple MVPs by reporting as part of a group for one pathway and as part of a subgroup for a different pathway. Beginning in the 2026 performance year, multispecialty groups will be required to form subgroups for MVP participation.
A subgroup is defined as one or more MIPS-eligible clinicians within a group practice. CMS has proposed that the Provider Enrollment, Chain, and Ownership System (PECOS) be used as the determinant of the specialty type for a single- or multispecialty group.
Participants will be required to register their reporting status between April 1 and November 30 of each performance year. At the time of registration, a participant will select the following:
- The MVP they intend to report
- One population health measure included in the MVP
- Any outcomes-based administrative claims measure on which the MVP participant intends to be scored if available within the MVP
Each subgroup will also be required to do the following:
- Identify the MVP on which the subgroup will report, including the population health measure and any administrative measure on which the subgroup intends to be scored.
- Identify the clinicians in the subgroup by Taxpayer Identification Number (TIN) and National Provider Identifier (NPI)
- Provide a plain language name for the subgroup for public reporting purposes.
A participant will not be allowed to submit or make changes to the MVP they have selected after the November 30 close of the registration period, and they will not be allowed to report on an MVP for which they did not register.
With all the rules for reporting and the options included, it will be challenging for providers to optimize their scores in 2023. Contact Healthmonix to gain insight on how to begin your reporting for 2023 and optimize results.

