As MACRA barrels into its second full year of implementation, we’re noticing mixed reactions to the reporting process. Some practices and organizations have thrown their best efforts into reporting and earning an incentive, while others are only interested in finding the easiest way to get compliant and avoid any penalty on their Medicare Part B reimbursements.
As MACRA barrels into its second full year of implementation, we’re noticing mixed reactions to the reporting process. Some practices and organizations have thrown their best efforts into reporting and earning an incentive, while others are only interested in finding the easiest way to get compliant and avoid any penalty on their Medicare Part B reimbursements.The question we get asked most often is: “What is the easiest way to report?” While there is no one-size-fits-all process for reporting, a great place to start is your Revenue Cycle Management.
RELATED: The Case For Reporting More Than The Minimum
Here are four reasons why the first steps in MIPS/MACRA compliance (and value-based care, in general) lies within your RCM:
 It affects your bottom line based on your Medicare Claims.
It affects your bottom line based on your Medicare Claims.
MACRA is going to affect the way your Revenue Cycle Management succeeds. It was designed to help resolve the Sustainable Growth Rate and eventually lead the push away from Fee for Service to Value-Based Care models. Put simply, MACRA is the first step towards restructuring the way practices receive revenue from Medicare. Any payment adjustment, positive or negative, for MIPS or previous PQRS reporting years will be seen in your Medicare reimbursements.
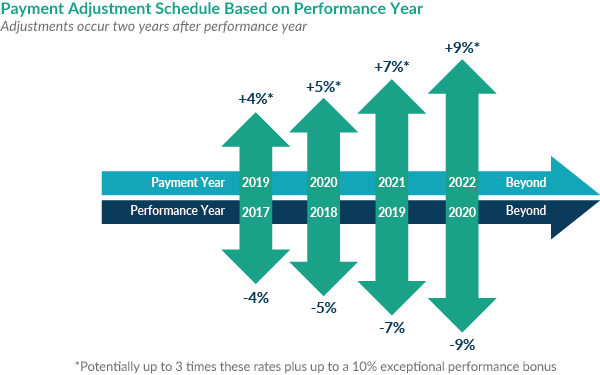
Knowing where your money is coming from will require at least a basic level of engagement with MACRA, and your revenue stream is the very best indicator you have of your performance. Keeping an eye on it and doing some analysis now empowers you to make the best choices for the future, when adjustments can be as high as 9 percent.
 It can be easily overlooked.
It can be easily overlooked.
In the world of healthcare, technology is overwhelming! We have AI, cloud-based solutions, and sophisticated tools to treat patients. At the very least people are likely to jump into their EHR in order to see how they’re doing in their Quality of care. It’s easy to see why most people ignore their RCM.
Doctors would rather treat people than worry about business considerations. The problem is, the consequences of non-compliance with MIPS and MACRA can sneak up on you because they aren't immediate. Those who are opting to not report in 2018 won’t see any negative adjustments until 2020. Once they are noticed in the revenue stream, it is virtually impossible to get those penalties reversed. You will be giving up 5% of your Medicare reimbursements for the 2020 calendar year, and will likely be scrambling to ensure you are doing what you need to for 2019 reporting year compliance.
If you don’t know now where your 2020 adjustment will lie, you’ll be playing catch up and feeling the sting until 2021. And that’s a shame, especially because…
 Your claims contain most of your quality data.
Your claims contain most of your quality data.
Most people asking me about reporting MIPS say they went straight to their EHR. While that may be a good litmus of what is and isn’t being tracked, your EHR is not the end-all for quality performance data. Practices and provider organizations are surprised to hear that most of the data they need to report successfully is contained within the very claims they bill to Medicare.
Every Quality measure is based on the CPT codes and Diagnosis codes billed to CMS. This means you can learn a lot about reporting from your claims. You can determine which measures make sense to report, which ones are the most common, how many instances and how much work will be required to report.
Practices are surprised to see that loading their claims to a registry can even show them some performance data or gaps in performance. There’s no reason to rely fully on your EHR when you can use the same data CMS uses to manage your reporting.
 It’s the most efficient way to tackle reporting.
It’s the most efficient way to tackle reporting.
As we transition from FFS to Value-Based Care, it’s no longer about the volume of patients—it’s about how efficiently we provide care for those patients. You don’t need to add new technology infrastructure, switch EHRs, or drastically change staffing and procedures to adjust to MACRA. You just need to use your existing resources in the optimal way.
By making your RCM the first stop in your journey to quality reporting compliance, you’re going directly to the core of your data. You’re seeing it without any filters and most closely aligned with the way these measures are written into MIPS. The best part of this is, you don’t need to change very much of anything to collect that data.
If you bill Medicare, you have eligible patients. If you use any office visit codes, you have eligible instances. If you can access any of that information, you have a starting point for MIPS. We don’t need to re-invent the continuum of care in order to be compliant and create positive effects on our bottom line and quality of care. For MIPS, start at the course and look to what’s contained in your RCM system. Once you recognize this, it’s easy to get your data into a MIPS Registry and get that CMS incentive.
There is a lot of nuance involved in reporting MIPS data in order to maximize reimbursements. With MIPSPRO, you don’t need to make any decisions until you are done gathering your data and are ready for final submission. MIPSPRO users are better equipped to choose the most advantageous reporting approach for their particular situation because they can base these choices on actual data as opposed to estimates, and because they are able to see estimated MIPS Scores based on each option, before final submission. Plus, our fabulous support staff will help guide you through the submission process so you can maximize your chances of reporting success. Find out how to get started today.