The Quality Performance Category
The Quality Performance Category is one of four Performance Categories to be reported for the Merit-Based Incentive Payment System (MIPS). Carrying the highest weight of the four Performance Categories, the Quality Score will determine 60% of the MIPS Composite Performance Score for eligible clinicians or groups.
Quality is closely related to its predecessor, the Physician Quality Reporting System (PQRS). Much Like PQRS, it can be reported individually or as a group, and requires submission of quality measure information to CMS.
Changes from PQRS
|
PQRS |
MIPS Quality Performance Category |
|
Report 9 Individual Measures |
Report 6 Individual Measures |
|
Measures cover 3 NQS domains |
No NQS Domain Requirement |
|
Measure groups are reportable |
No measure groups available, specialty measure sets |
|
Report 50% of eligible instances for Medicare Part B patient visits |
Report 50% of eligible instances across all payers |
|
One cross-cutting measure |
One outcome or "high priority" measure |
How to Report the MIPS Quality Performance Category
 Determine MIPS Eligibility and Level of Reporting (TIN or NPI)
Determine MIPS Eligibility and Level of Reporting (TIN or NPI)
The first step to MIPS reporting is determining if you need to report, and if you will be reporting on a group (TIN) or individual (NPI) level. Physicians, Physician Assistants, Nurse Practitioners, Clinical Nurse Specialists, Certified Registered Nurse Anesthetists are all considered eligible clinicians in 2017. MIPS reporting will be required for eligible clinicians who are not participating in an Advanced Alternative Payment Model, see at least 100 Medicare Part B beneficiaries, and at have at least $30,000 in Medicare Part B allowed charges.
Whether you report as a group or as an individual, you must do so for every performance category of MIPS. Groups will be determined on the TIN level, and may contain all clinicians that would otherwise be considered ineligible.
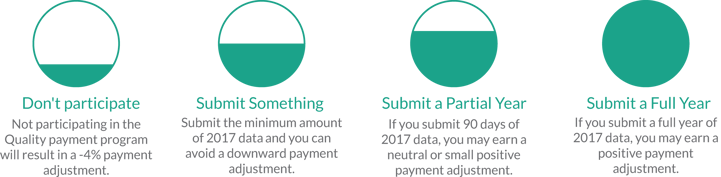
 Determine level of participation
Determine level of participation
You have an option of reporting 1 Quality Measure to avoid the MIPS penalty, or reporting up to 6 Quality Measures to get an incentive payment. Additionally, you can choose to report for as little as a 90-day consecutive period, or for the entire performance year. The more you report, the higher incentive you will be eligible for.
 Select Measures
Select Measures
The Quality measures for MIPS are the same measures that were used for PQRS, with a few changes and additions. For easy measure selection, you can search through pre-determined recommended measures for your specialty.
When selecting measures to report, first select your outcome measure. If no outcome measure is available to report, you can select a high-priority measure in its place. For each additional outcome measure reported past the first required outcome measure, you can recieve 2 bonus points. For each additional high-priority measure, you can recieve 1 bonus point. After you have selected all of the outcome and high-priority measures you want to report, select other applicable measures until you have at least 6 measures.
If you are using electronic reporting or another mechanism that allows for easy measure tracking, we recommend tracking all applicable measures. When you submit your measure data, CMS will accept the highest performing measures and disregard the rest!
Keep in mind that this year you must report 50% of the eligible instances for each measure across all payers. This is a significant change from PQRS, which was only for Medicare Part B beneficiary visits. In the upcoming years, the reporting rate will gradually increase from 50% to 90%.
 Review Data & Submit!
Review Data & Submit!
Your MIPS Quality Performance Category score will be determined based on benchmarks obtained from a prior performance year. MIPSPRO integrates these benchmarks into your dashboard, allowing you to anticipate your performance in real-time.