The 2018 Quality Payment Program proposed rule suggests significant changes to MIPS reporting. The changes proposed are aimed at easing the burden of reporting while increasing the meaningfulness of compliance. We have previously discussed new policies being introduced and changes compared to 2017 reporting. The 2018 proposed rule also suggests changes to the MIPS Performance Categories.
Quality Performance Category
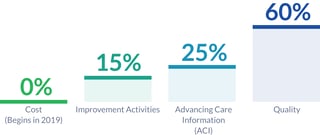
The Quality Performance Category is proposed to continue to be weighted as 60% of the MIPS final score for the performance years of 2018 and 2019, and its worth reduces to 30% of the MIPS final score in the performance year of 2020. This is a change from the gradual reduction in weight suggested in the 2017 final rule.
Additionally, the data completeness criteria will remain unchanged for the 2018 performance year at 50% of all payers for every submission mechanism besides the CMS web interface and CAHPS instead of increasing to 60% as previously suggested. CMS still plans to increase the data completeness threshold to 60% for the 2019 performance year. The MIPS "Pick Your Pace" option will also be changed, allowing clinicians one point for measures that do not meet data completeness criteria instead of three. The exception to this will be small practices (15 or fewer clinicians), who will continue to get three points.
CMS will also begin to identify six measures per year that will be considered "topped-out," meaning these measures consistently have very high performance rates. The "topped-out" measures will be capped at six points rather than ten, and will be retired after three years. This will challenge clinicians to explore bridging new gaps in care, rather than relying on reporting the same measures that are commonly met with success.
CMS will also incentivize year-over-year improvement in performance. They will compare MIPS eligible clinicians' and groups' performance to the performance achieved in the prior performance period, for up to ten additional Quality Performance Category points.
Cost Performance Category
The Cost Performance Category is worth 0% the MIPS final score for the 2017 performance year, although eligible clinicians or groups can request a feedback report to see how they would have performed in this category. At this point in time, CMS is proposing to keep the weight of Cost at 0% for the 2018 performance year, but is specifically requesting feedback surrounding the idea of increasing the weight to account for 10% of the MIPS final score. If the Cost Performance Category is given a weighting above 0%, it will also incentivize performance improvement in a similar way to the Quality Performance Category.
Improvement Activities Performance Category
The Improvement Activities Performance Category will continue to be weighted at 15% of the MIPS final score. Additionally, the required number activities will not change. CMS is proposing additional Improvement Activities to add to the 92 that exist for the 2017 performance year, more of which will be eligible for ACI Performance Category bonus points.
CMS is updating the definition of a patient-centered medical home to include the CPC+ APM model, allowing practices participating in this type of APM to be automatically awarded full credit in the category score, rather than half. Otherwise, the category will likely remain largely unchanged.
Advancing Care Information Performance Category
In the 2017 final rule, CMS stipulated that eligible clinicians and groups should plan to have 2015 edition CEHRT to expect to be able to satisfy ACI requirements for the 2018 performance year. This requirement is proposed to be postponed, allowing 2014 edition CEHRT to participate. However, having 2015 edition CEHRT and reporting fully through it will award ACI bonus points.
More exclusions are also proposed. MIPS clinicians who are based in an ambulatory surgical center (ASC-based), small practices (15 or fewer clinicians), and clinicians who have had their CEHRT decertified will be added to the list of MIPS clinicians eligible to have ACI re-weighted to 0%. The 25% of the MIPS final score that would be from ACI would be reallocated to the Quality Performance Category. Exclusions will also be added for the E-Prescribing and Health Information Exchange measures.
With this proposal, CMS intends to achieve improved health outcomes, wiser spending, a minimal reporting burden, and a fair and transparent system. If you have comments or feedback about these proposals, you should weigh in before August 18, 2017. Comments can be made through mail or electronically through regulations.gov, referencing file code CMS 5522-P.
Citations:
[1] Unpublished Proposed Rule: Medicare Program; CY 2018 Updates to the Quality Payment Program
[2] Quality Payment Program Proposed Rule Fact Sheet