In 2025, Medicare introduced three new Advanced Primary Care Management (APCM) codes —G0556, G0557, and G0558 — to support streamlined, comprehensive care for patients with chronic conditions. These codes not only simplify billing but are also tied to performance reporting under the Merit-based Incentive Payment System (MIPS). This post breaks down what providers need to know.
Simplifying chronic care: What you need to know about APCM codes and MIPS MVP reporting
Topics: Quality Performance Category
Transforming care through collaboration: Lessons from the frontlines of value-based healthcare
One theme emerged loud and clear at the NAACOS Spring 2025 Conference: transformation isn’t just about systems. It’s about people, collaboration, and actionable workflows.
Healthcare organizations nationwide are navigating the complexities of value-based care (VBC). VBC success is measured in procedures performed and outcomes achieved. It requires coordination between technology, teams, and providers.
Many organizations are struggling to close the gaps.
Topics: Quality Performance Category
Redesigning the system: A narrative from Becker’s 2025 annual meeting
Last week, I had the opportunity to join healthcare executives, clinical leaders, and innovators from across the country at the Becker’s Hospital Review 15th Annual Meeting. Every year, this event captures the current temperature of healthcare transformation — but this year felt different. There was a sharpened urgency in the air and a deeper willingness to challenge long-standing norms.
Across sessions, one question echoed consistently: How do we design a healthcare system that truly delivers value — to patients, providers, employers, and communities?
Topics: Quality Performance Category
The Transforming Episode Accountability Model (TEAM): A new era in healthcare
The Transforming Episode Accountability Model (TEAM) is set to revolutionize how hospitals coordinate care for Medicare beneficiaries undergoing high-risk, high-volume surgical procedures. Slated to start in January 2026, this 5-year, mandatory model will focus on improving patient care quality while controlling costs.
Here’s an in-depth look at what TEAM entails and its potential to transform the healthcare landscape.
Topics: Quality Performance Category
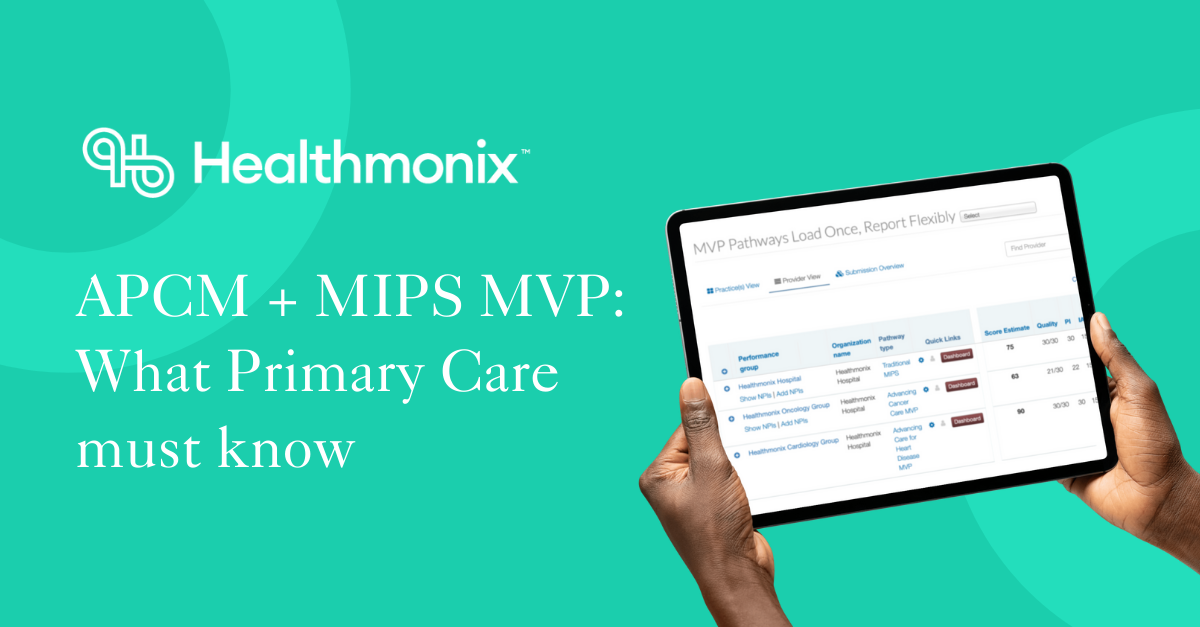
What primary care providers must know about billing, compliance, and MIPS MVPs in 2025
In 2025, CMS launched a significant evolution in its commitment to primary care: the Advanced Primary Care Management (APCM) codes. These codes — G0556, G0557, and G0558 — are designed to simplify billing, support patient-centered care, and advance health equity for patients with chronic conditions.
But there’s a catch. These codes come with new requirements, including participation in the Value in Primary Care MIPS Value Pathway (MVP) for eligible clinicians.
In this post, we’ll break down:
- What APCM codes are
- Who can bill them
- How they differ from existing care management codes
- What’s required for MIPS compliance
- What happens if you don’t report
- What steps your practice should take next
Topics: Quality Performance Category
Healthmonix has done it: Quality reporting success for MSSP ACOs at scale
As value-based care matures, MSSP ACOs face mounting complexity in quality reporting — across EHRs, payers, and evolving CMS requirements. At Healthmonix, we don’t just promise solutions. We’ve already delivered them — at scale, across diverse ACOs, and in direct partnership with forward-thinking healthcare leaders.
Topics: ACO, Quality Performance Category
MIPS Cost scores are coming — what to know for 2024 and prepping for 2025
If you’re an eligible clinician participating in MIPS, your 2024 Cost category score will be calculated after submission — and the results may come as a surprise. With Cost accounting for 30% of your total MIPS score, it’s no longer an afterthought. It’s a major factor in your final performance.
Topics: MIPS Reporting
Healthmonix’s EACCR designated as a 2025 Qualified Clinical Data Registry by CMS
Malvern, Pa. —Healthmonix is proud to announce that the Emergency and Acute Care Clinical Registry (EACCR) has been approved as a Qualified Clinical Data Registry (QCDR) by the Centers for Medicare & Medicaid Services (CMS) for the 2025 reporting year. This is the fifth straight year Healthmonix has earned this designation for EACCR, which empowers clinicians to seamlessly meet Merit-based Incentive Payment System (MIPS) requirements while leveraging innovative tools to drive improvements in patient care and streamline regulatory compliance.
Topics: MIPS Reporting
Healthmonix unveils 2025 Mental and Behavioral Health Registry (MBHR) with key measures to enhance care delivery
Malvern, Pa. (Jan. 20, 2025) — Healthmonix is proud to announce the release of the 2025 Mental and Behavioral Health Registry (MBHR), a specialized Qualified Clinical Data Registry (QCDR) developed with the American Psychological Association to improve care for individuals with mental and behavioral health conditions. This registry provides healthcare providers with essential tools to track, report, and optimize clinical outcomes in the treatment of mental health and behavioral disorders.
Topics: MIPS Reporting
Healthmonix launches 2025 MIPSpro Enterprise QCDR, expanding support for key healthcare specialties
Malvern, Pa. (Jan. 13, 2025) — Healthmonix is proud to announce the release of the 2025 MIPSpro Enterprise Qualified Clinical Data Registry (QCDR). We’ve updated this cutting-edge registry to provide comprehensive support for a wide range of healthcare specialties, helping providers improve care quality, achieve regulatory compliance, and drive better patient outcomes across various clinical settings.
Topics: MIPS Reporting