On Tuesday April 24th, CMS released a proposed rule which essentially overhauls the Medicare and Medicaid Electronic Health Record Incentive Programs (also known as the “Meaningful Use” program). The proposed rule includes updates to Medicare payment policies and rates under the Inpatient Prospective Payment System (IPPS) and the Long-Term Care Hospital (LTCH) Prospective Payment System (PPS). Here are five things you should know about the proposed changes:
Christina Zink
Recent Posts
CMS Proposes Overhauling Meaningful Use: 4 Important Takeaways
Topics: CMS, Interoperability, Policy, ACI Performance Category, PI Performance Category
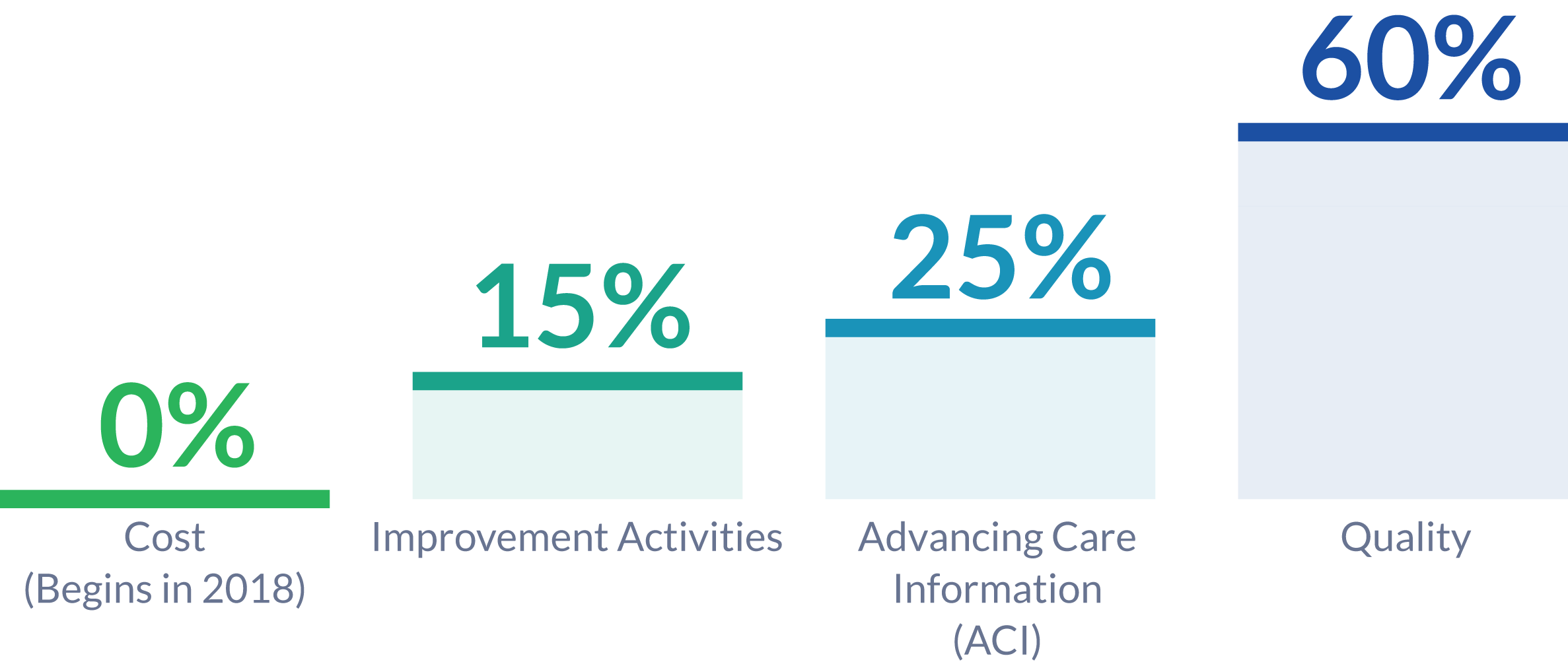
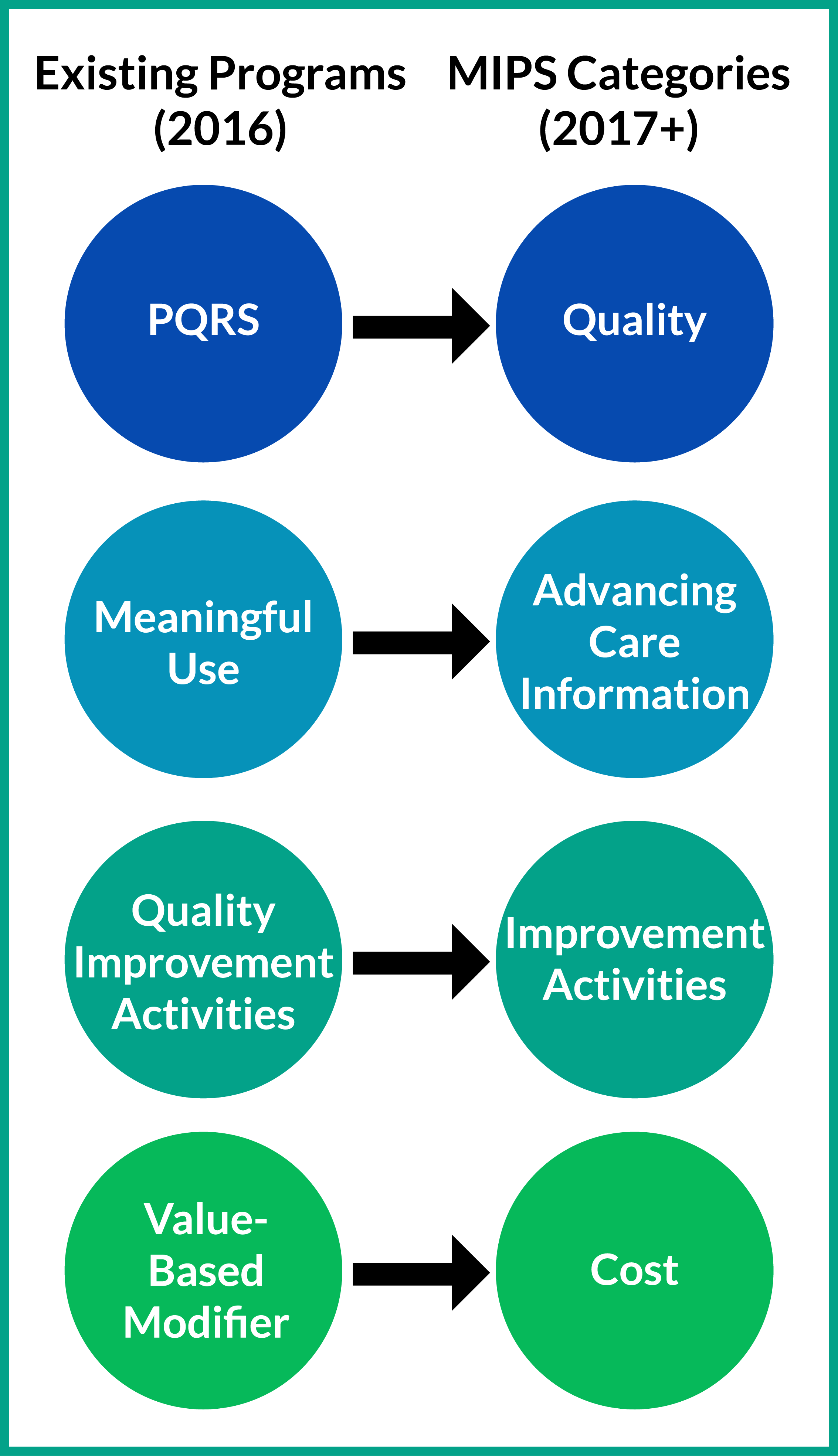
With the first performance year of the Merit-based Incentive Payment System (MIPS) drawing to a close, you may have just started getting accustomed to how MIPS reporting works. Although the 2018 MACRA final rule introduced changes to how MIPS performance data should be captured for the upcoming performance year, it may be a relief to hear that largely the changes just build upon the existing 2017 regulations.
Topics: MACRA & MIPS, Policy, Quality Performance Category, ACI Performance Category, IA Performance Category, Cost Performance Category
Yesterday afternoon, CMS released the 2018 Final Rule for the MACRA Quality Payment Program. The rule finalized some changes we were expecting, and others that came as a surprise. The second year of the Quality Payment Program will be more advanced than the first, aiming to get clinicians ready for the even more intense requirements mandated by the MACRA legislation to be enacted in 2019.
Topics: MACRA & MIPS, Policy
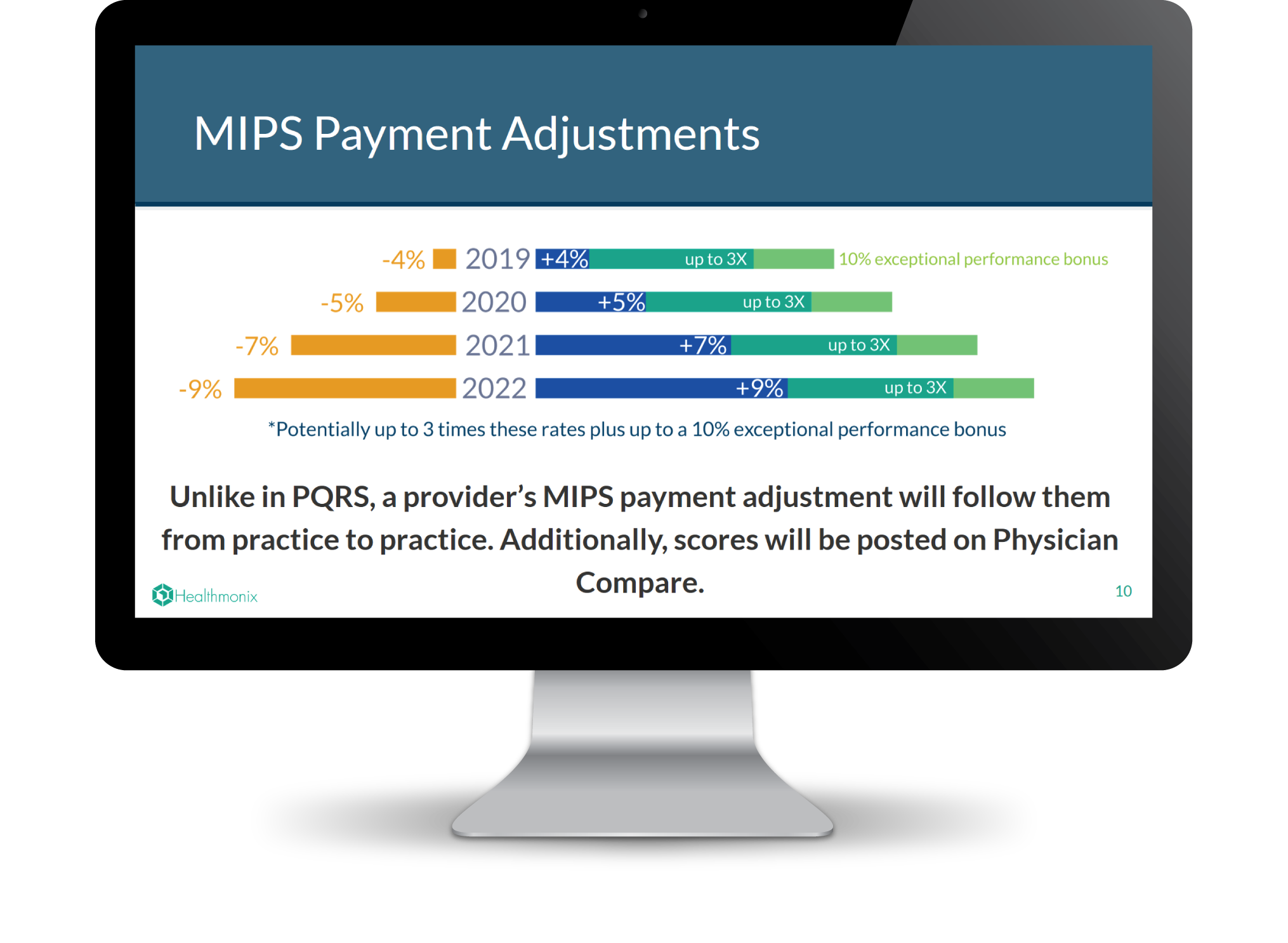
To prosper in an industry challenged by constantly changing reform and increasing competition, healthcare organizations must continually increase their quality of care and become more efficient. Reporting MIPS in 2017 is a low-risk, high reward condition to stress-test your clinical workflows for optimized value-based program reporting.
Topics: MACRA & MIPS, Policy
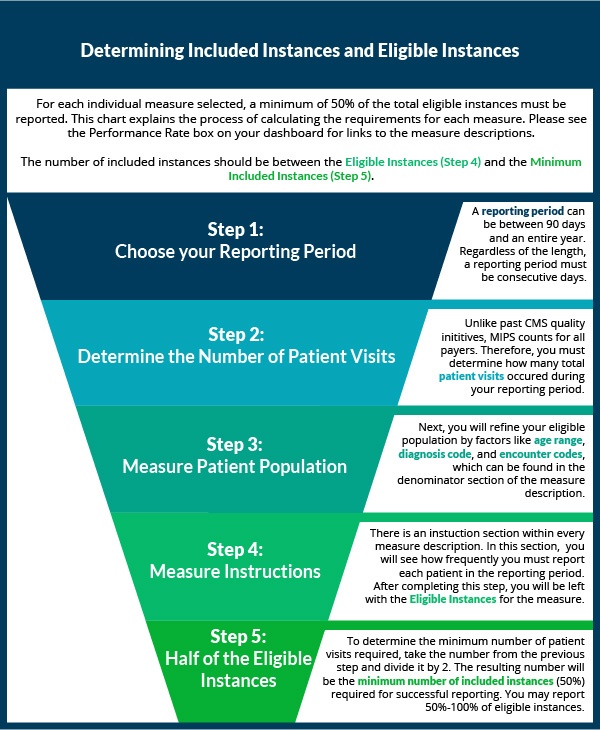
Data Completeness for MIPS Quality Measures [Infographic]
Over the last two weeks, we've shown you how to select quality measures. Now that you've decided which measures to collect data for, it's time to start reporting! If you have reported PQRS in the past, the process will be similar with a few major changes. Eligible clinicians who are new to reporting may want to first check out our article on the basics of quality measures prior to understanding how to completely report a quality measure.
Topics: MACRA & MIPS, Policy, Quality Performance Category
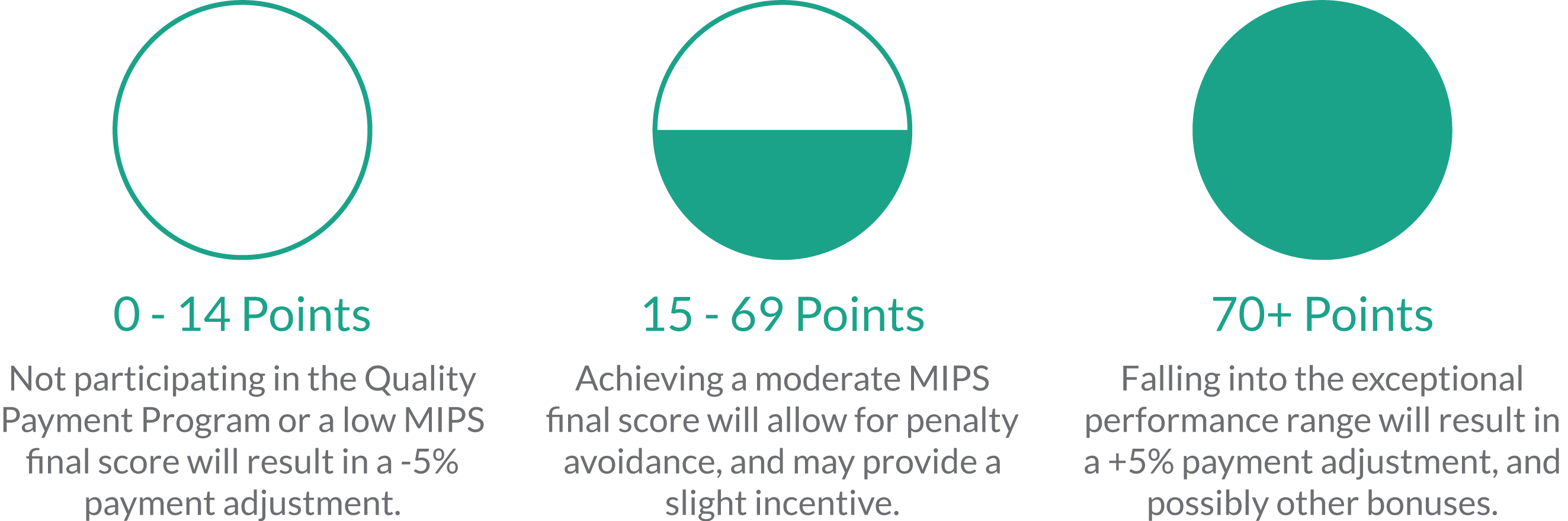
We are now in the seventh month of the new Merit-Based Incentive Payment System (MIPS), and the majority of MIPS-eligible clinicians still feel completely unprepared for success. With complicated and changing regulations, ensuring compliance can be a long and arduous process. Like most sizable goals, MIPS is best digested in small pieces, but it is hard to tell where to start sometimes. That is why we are going give you an order of operations to follow to ensure MIPS survival.
Topics: PRO Tips, MACRA & MIPS, CMS, Eligibility
The 2018 Quality Payment Program proposed rule suggests significant changes to MIPS reporting. The changes proposed are aimed at easing the burden of reporting while increasing the meaningfulness of compliance. We have previously discussed new policies being introduced and changes compared to 2017 reporting. The 2018 proposed rule also suggests changes to the MIPS Performance Categories.
Topics: MACRA & MIPS, Policy
The 2018 MIPS Proposed Rule was just released by CMS, and it contains changes from the 2017 rule which providers may benefit from considering in relation to their reporting goals and strategies. In our last post we outlined various new proposals as well as new opportunities for bonus points in the MIPS final score. Here we clarify further changes from 2017, including updates on the low volume threshold, submission options, and the minimum performance period.
Topics: MACRA & MIPS, Policy
Yesterday afternoon, CMS posted CY 2018 Updates to the Quality Payment Program to the Federal Register, to be officially published at the end of this month. Many clinicians are still trying to wrap their heads around how to report MIPS in 2017. However, the release of the 2018 proposed rule is advantageous as aid deciding what to conquer in 2017, and which aspects of MIPS can be digested in the future. As the title suggests, this document also covers other Quality Payment Program tracks, like Advanced APMs. As the vast majority of healthcare providers are expected to be participating in MIPS for 2017 and 2018, we are just going to focus on the MIPS component of the proposed rule for now.
Topics: MACRA & MIPS, Policy
With the beginning of June came the half-way point for the first year of MIPS reporting. While many providers haven't started reporting yet, a good number of clinicians have started early. We interviewed clinicians and practice administrators who have reported PQRS in the past via registry, are currently reporting through the MIPSPRO registry, and that represent a diverse demographic of MIPS eligible clinicians.
Topics: PQRS, MACRA & MIPS, Industry insights, Small Practice, Hospitals & Health Systems