Thanksgiving is almost here! For me, this means reflecting on the things in my life that I am thankful for. Along with the tasty food I am about to consume with my loved ones, this year I am grateful for the MACRA Quality Payment Program. This may sound perplexing to you, as the MACRA Quality Payment Program has been causing a lot of alarm in the healthcare industry since the Notice of Proposed Rule Making (NPRM). However, with the release of the final rule came many provisions that I believe will improve the ease of reporting for clinicians while continuing to improve the quality of care for patients.
To briefly refresh before jumping in, the MACRA Quality Payment Program is split into two paths: the Merit-Based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (Advanced APMs). MIPS streamlines pre-existing CMS quality initiatives (like PQRS and Meaningful Use), while Advanced APMs are designed to encourage innovative value-based payment models.
 Penalty Avoidance Just Got Much Easier
Penalty Avoidance Just Got Much Easier
Prior to the release of the final rule, CMS Acting Administrator, Andy Slavitt, announced that there would be transitionary "pacing" options available for the first year of MIPS. With the release of the final rule, we got to see just how easy avoiding the MIPS penalty will be in 2017 with the elaboration of these transition year options.
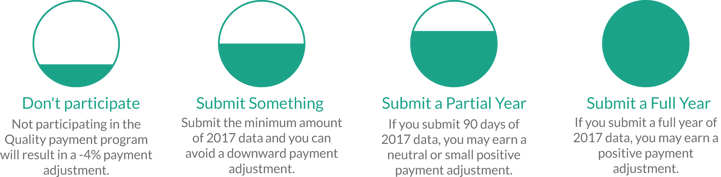
In order to avoid the -4% adjustment to your Medicare Part B claims in 2019, all that must be reported in 2017 is one (1) quality measure OR one (1) improvement activity OR the five (5) required Advancing Care Information measures. Considering that some improvement activities may already be common practice in your organization (for example, tobacco use screening and cessation interventions), and all that is required is an attestation improvement activities, the reporting burden has been significantly reduced when compared to 2016 reporting activities for PQRS/MU.
 Incentives are Back with a Vengeance
Incentives are Back with a Vengeance
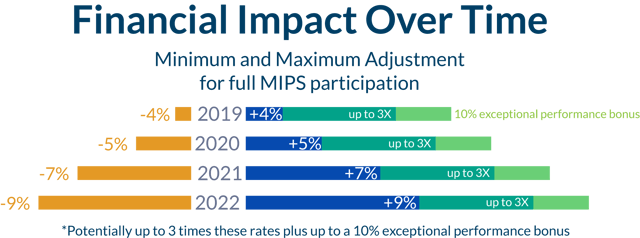
With 2015 PQRS reporting, providers stopped being able to receive incentives based on their PQRS quality reporting. For the Merit-Based Incentive Payment System (MIPS), maximum incentives will start at 32% for performance year 2017 (payment year 2019) and gradually ramp up to 37% by performance year 2020 (payment year 2022).
 Education and Support for the Quality Payment Program
Education and Support for the Quality Payment Program
As specified in the strategic objectives for the Quality Payment Program, a primary goal of the program is to "promote program understanding and participation through customized communication, education, outreach, and support." [2] For small and rural practices, a budget for support has been written into the legislation for MACRA:
"In keeping with the objectives of providing education about the program and maximizing participation, and as mandated by the MACRA, $100 million in technical assistance will be available to MIPS eligible clinicians in small practices, rural areas, and practices located in geographic health professional shortage areas (HPSAs)..." [2]
- MACRA Quality Payment Program Final Rule, p. 77012
CMS is already making good on this promise. The new Quality Payment Program website is a vast improvement when compared to the information available for PQRS, the EHR Incentive Payment, or the Value-Based Payment Modifier. On the day they released the final rule, they also released a fact sheet covering how and where to get help with program support.
 Innovative Payment Models are Now Being Encouraged
Innovative Payment Models are Now Being Encouraged
In the 2017 performance year, satisfactory participation in select APMs, referred to as Advanced Alternative Payment Models (Advanced APMs), will result in an automatic 5% incentive. To satisfactorily participate in an Advanced APM, a clinician must demonstrate that either 25% of Medicare payments are through an Advanced APM OR 20% of Medicare patients are through an Advanced APM.
CMS anticipates that by the performance year of 2018, 50% of MACRA Quality Payment Program participants will be participating through an Advanced APM. For the performance years of 2017 and 2018, incentive payments are restricted to Medicare patients. However, starting with performance year 2019 clinicians will also be able to meet Advanced APM standards with non-Medicare patients. This will theoretically help align the incentives available through Medicare with incentives that will be offered by other payers as the industry continues to shift to value-based care.
 MACRA is Inspiring HIT to become Fully Interoperable
MACRA is Inspiring HIT to become Fully Interoperable
Another strategic goal of the MACRA Quality Payment Program is to "improve data and information sharing to provide accurate, timely, and actionable feedback to clinicians and other stakeholders." [2] On November 17, CMS announced one way in which they are going to help facilitate that end.[3] CMS is providing Application Program Interfaces (APIs) that will allow your Certified EHR Technology (CEHRT) to directly interface with CMS's measure specifications.
This is a huge deal, because one of the main issues that providers have been having when trying to complete quality reporting through CEHRT was incorrectly programmed measure specifications. This interferes with you receiving the credit you deserve for your quality reporting. The increased dependability of CEHRT will begin to enable providers to be able to capture quality data as it is entered into a chart, rather than having to separately enter it into a quality reporting mechanism.
As a secondary bonus, this level of ease regarding measure programming will free up your CEHRT vendors to innovate products to make them more user-friendly and powerful. Speaking as someone who works in a CEHRT company, I understand that a great deal of time, energy, and attention goes into ensuring that the measures we provide are accurately represented in our systems. We are excited for this process to be automated so we can provide a more exceptional user experience!
Citations
[1] The Department of Health and Human Services. (2016, Oct. 14). Executive Summary; Medicare Program; Merit-based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Incentive under the Physician Fee Schedule, and Criteria for Physician-Focused Payment Models. Retrieved from https://qpp.cms.gov/docs/QPP_Executive_Summary_of_Final_Rule.pdf
[2] Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Final Rule, 42 CFR § 414 (2016). [CMS-5517-FC]
[3] The Centers for Medicare and Medicaid Services. (2016, Nov 17). CMS launches new online tool to make Quality Payment Program easier for clinicians [Press Release]. Retrieved from https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2016-Press-releases-items/2016-11-17.html
