To prosper in an industry challenged by constantly changing reform and increasing competition, healthcare organizations must continually increase their quality of care and become more efficient. Reporting MIPS in 2017 is a low-risk, high reward condition to stress-test your clinical workflows for optimized value-based program reporting.
CMS is worried about how few providers understand or are even aware of MACRA. As we near October 2nd, the deadline by which 400,000 eligible providers must start tracking data in order to avoid a financial penalty in 2019, CMS has found that around 40% of clinicians and even fewer nurse practitioners have a solid understanding of the requirements. Their concern is only supported by a recent Integra Connect survey which finds that most specialty physicians have not yet made the operational changes necessary to succeed in the new world of value based care.
Topics: MACRA & MIPS
Statistically, you aren’t sure how you’re supposed to comply with quality reporting requirements this year. As late as June 2017, the majority of providers were still unfamiliar or only somewhat familiar with MACRA; only 9 percent described themselves as “very familiar”. But unless you’re a part of that 9 percent, we highly recommend that you take some time ASAP to familiarize yourself with the requirements and to make a plan for the rest of the year. And as part of that plan, here are four reasons why we recommend that you select Improvement Activities for your practice today (yes, literally today):
Topics: PRO Tips, MACRA & MIPS, IA Performance Category
Data Completeness for MIPS Quality Measures [Infographic]
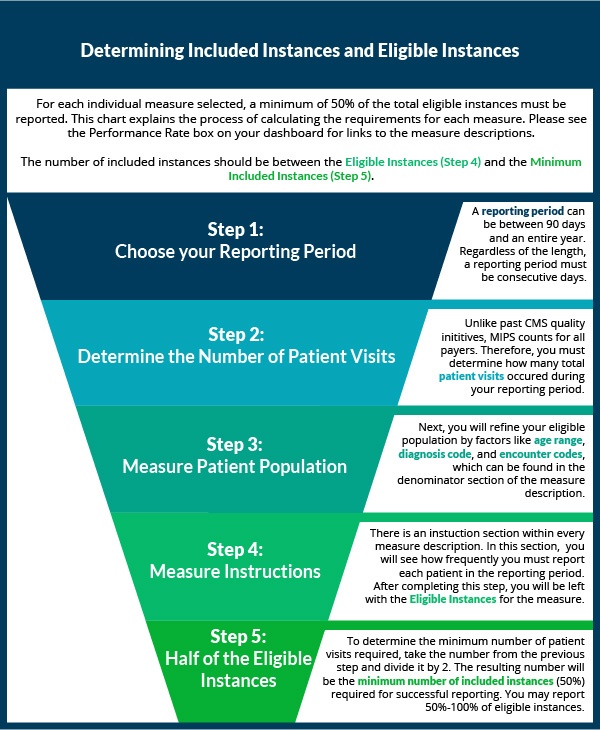
Over the last two weeks, we've shown you how to select quality measures. Now that you've decided which measures to collect data for, it's time to start reporting! If you have reported PQRS in the past, the process will be similar with a few major changes. Eligible clinicians who are new to reporting may want to first check out our article on the basics of quality measures prior to understanding how to completely report a quality measure.
Topics: MACRA & MIPS, Policy, Quality Performance Category
In our last post, we covered some of the basic questions you should be asking yourself when choosing quality measures to report under MIPS. In part two of this series, we go over a few more specific questions that can help guide you to picking the best measures for your practice.
Topics: MACRA & MIPS, Policy, Quality Performance Category
So you’re a MIPS-eligible clinician (if you’re not sure about your participation status, check out our post about how to find out), and you don’t want your practice to miss out on the reimbursement you know you deserve. But how should you decide which quality measures to actually report to CMS? How can you know if the measures you’re choosing will ultimately lead to reporting success, and is there a way to use those measures to not just fulfill the requirements but actually improve your practice? We’ve put together a two-part post to guide you through the most important factors to consider when deciding what might be best for you and your practice. First, the basics:
Topics: MACRA & MIPS, Policy, Quality Performance Category
 The shift from volume to value-based care can be frustrating, especially when the reasons behind such a significant change aren’t clear. But with an estimated 250,000 American deaths per year caused by medical errors, minimizing these errors is a noble and vital effort. Additionally, CMS is now raising the bar for healthcare providers with the assessment of quality metrics against benchmarks and peers. With that in mind, let’s break down the meaning of, and intentions behind, Quality Measures.
The shift from volume to value-based care can be frustrating, especially when the reasons behind such a significant change aren’t clear. But with an estimated 250,000 American deaths per year caused by medical errors, minimizing these errors is a noble and vital effort. Additionally, CMS is now raising the bar for healthcare providers with the assessment of quality metrics against benchmarks and peers. With that in mind, let’s break down the meaning of, and intentions behind, Quality Measures.
Topics: MACRA & MIPS, Policy, Quality Performance Category
Three Ways to Check Your MIPS Participation Eligibility Status
When we asked MIPS eligible clinicians about their experiences transitioning from PQRS this year, one of the biggest takeaways was that quality matters even more under MIPS than it did under PQRS. Clinicians who want to maximize their reimbursement would consequently be very smart to start reporting as early as possible, and to adjust performance to maximize quality, rather than waiting until the end of the year. If you’re not sure whether or not you are a MIPS-eligible clinician, take advantage of one of the following resources for determining your MIPS participation status as soon as possible so that you don’t get left behind.
Topics: PRO Tips, MACRA & MIPS, Eligibility
On Monday night this week, in the wake of news that there might not be enough votes to pass the updated Senate version of the AHCA, Senate Majority Leader Mitch McConnell (R-KY) announced a plan to vote for legislation that would repeal most of Obamacare without immediately putting an alternative in place. The alternative plan would instead be developed over the course of the next two years.
Topics: Policy
We are now in the seventh month of the new Merit-Based Incentive Payment System (MIPS), and the majority of MIPS-eligible clinicians still feel completely unprepared for success. With complicated and changing regulations, ensuring compliance can be a long and arduous process. Like most sizable goals, MIPS is best digested in small pieces, but it is hard to tell where to start sometimes. That is why we are going give you an order of operations to follow to ensure MIPS survival.
Topics: PRO Tips, MACRA & MIPS, CMS, Eligibility