The first performance year of the Merit-based Incentive Payment System (MIPS) is well underway. One of the most marked differences between MIPS and previous CMS initiatives is the quality of educational resources available to eligible clinicians. However, wading through all the different documents can be confusing if you are just starting out. This article will walk you through the available resources for each step of your MIPS educational journey.
House Republicans narrowly passed their long-promised Affordable Care Act repeal and replacement bill this Thursday. The American Healthcare Act barely scraped by with a vote of 217-213, with all 2017 "yes" votes coming from Republican Representatives. Although 20 Republican Representatives still opposed the bill, the revisions were able to convert 23 hard line conservatives into voting favorably. This proved enough for passage.
Topics: Policy
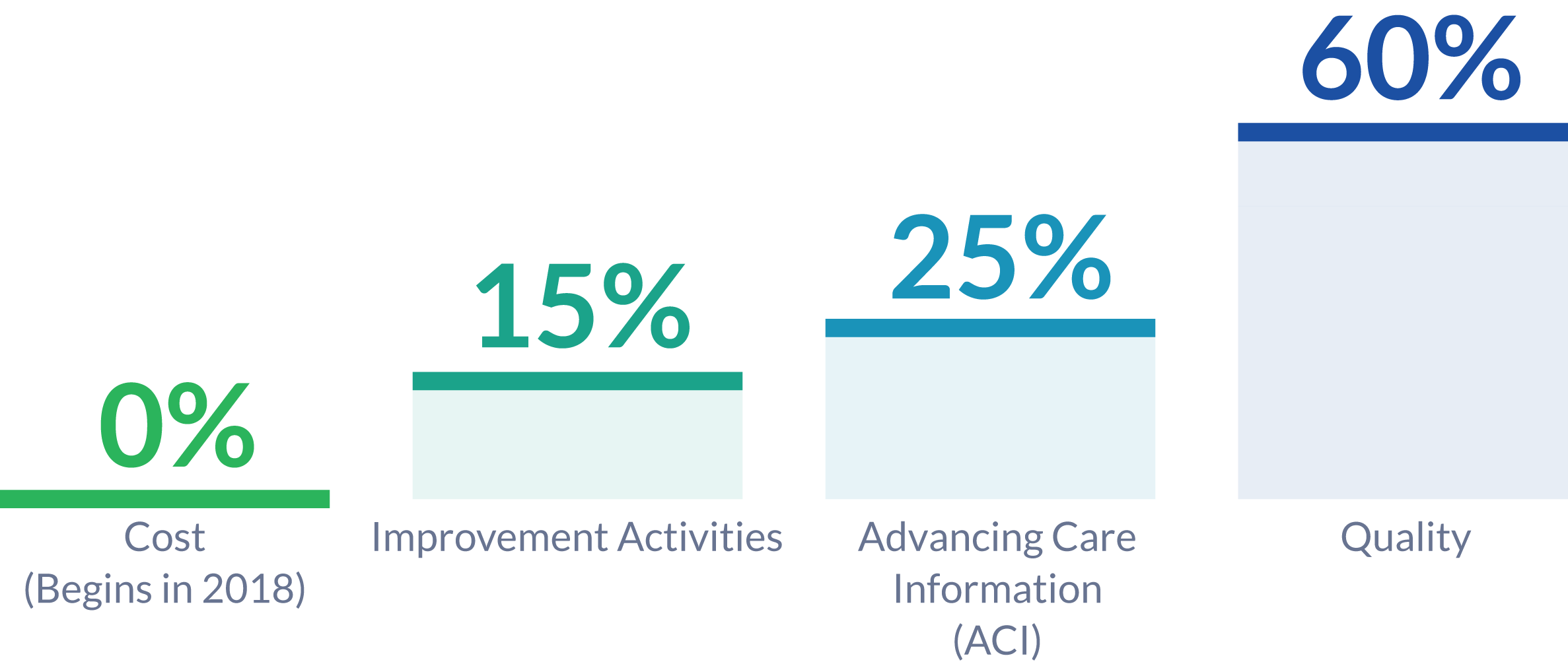
The Improvement Activities Performance Category is a new concept introduced by MIPS reporting and rewards eligible clinicians for participating in activities related to their patient population. Clinicians and groups can choose to participate in activities most relevant to both their practice and patient population. The Improvement Activities Performance Category is worth 15% of the MIPS Composite Performance Score in 2017.
Topics: MACRA & MIPS, Policy, IA Performance Category
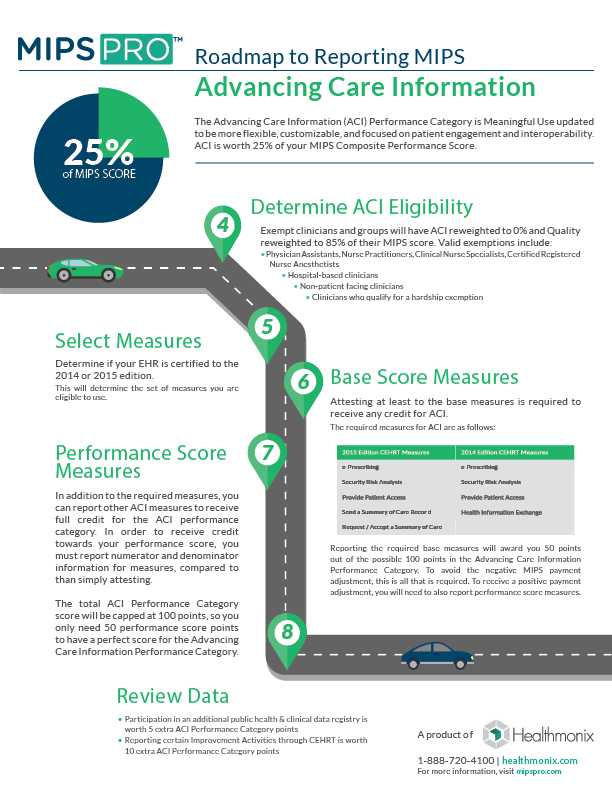
The Advancing Care Information (ACI) Performance Category is Meaningful Use updated to be more flexible, customizable, flexible and focused on patient engagement and interoperability. ACI is worth 25% of your MIPS Composite Performance Score.
Topics: MACRA & MIPS, Policy, ACI Performance Category
The Quality Performance Category
The Quality Performance Category is one of four Performance Categories to be reported for the Merit-Based Incentive Payment System (MIPS). Carrying the highest weight of the four Performance Categories, the Quality Score will determine 60% of the MIPS Composite Performance Score for eligible clinicians or groups.
Topics: MACRA & MIPS, Policy, Quality Performance Category
Although the president has stated that he is moving on to other issues, the GOP remains hopeful that they will dismantle and replace the Affordable Care Act (ACA) in the not-too-distant future. The Republican's proposed replacement bill, the American Health Care Act (AHCA) was withdrawn last Friday as it lacked the votes to pass. Under pressure from conservative activists this week, House Republicans and the White House have renewed their efforts to repeal the Affordable Care Act and replace it with their own bill.
Topics: Policy
MIPSPRO by Healthmonix Awarded 2017 Qualified MIPS Registry Status by CMS
Malvern, PA – March 16, 2017 – Healthmonix was first-to-market with an all-inclusive solution for MIPS reporting, MIPSPROTM. This Qualified MIPS Registry is an end-to-end reporting solution, supporting the Quality, Advancing Care Information, and Improvement Activity Performance Categories of the Merit-Based Incentive Payment System (MIPS). The MIPSPRO engine also provides sophisticated real-time performance analytics, critical to competing for top MIPS incentives and improving patient outcomes.
Topics: MACRA & MIPS, CMS, Healthmonix
This week, house Republicans introduced the long-anticipated Obamacare replacement plan. This plan, called the American Healthcare Act (AHCA), has received a high level of criticism already from a surprising mix of people. Although it certainly is too soon to tell, it seems as if the bill will likely not pass before significant edits are made.
Topics: Policy
HIMSS is the seminal event in healthcare technology each year. This year it grew to 45,000 attendees and literally a mile of exhibit hall. We logged miles of walking in one day just to cover the exhibit floor, and still did not see it all. At this pivotal time in healthcare information technology, there were many important themes that were covered.
Topics: Interoperability, Industry insights, Health IT
Compared to the commotion surrounding other Trump administration nominees, Seema Verma's confirmation hearing passed by last Thursday with relatively little controversy. Despite the low level of coverage, understanding the contents of this hearing is imperative for predicting the next few years in American health care. As the Administrator for the Centers for Medicare and Medicaid Services (CMS), Seema Verma will shape the future of health care for 34% of Americans. [1]
Topics: MACRA & MIPS, CMS