Early on the morning of February 10th, the Senate approved the nomination of now-former Rep. Tom Price to be the Secretary of Health and Human Services. While some say his chief priority is “dismantling of the Affordable Care Act” (Sen. Maria Cantwell of Washington), the tasks that will be put in front of him also include five major health IT initiatives: appointments to ONC and other agencies, the future of MACRA and Meaningful Use, the enforcement of interoperability, telemedicine, and cybersecurity.
The future of MACRA with Tom Price as the Secretary of HHS
Topics: MACRA & MIPS, CMS, Industry insights
Scoring the MIPS Advancing Care Information (ACI) Performance Category in 2017
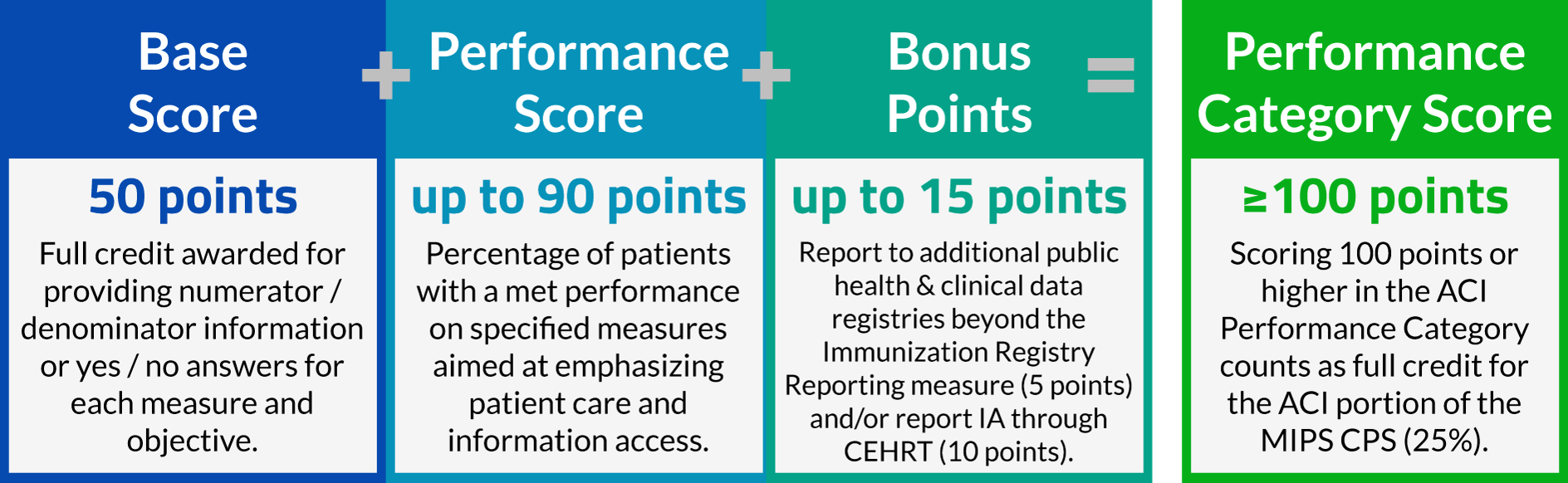
The Advancing Care Information Performance Category will be replacing the EHR Incentive Program (colloquially known as Meaningful Use) for 2017 performance year, as a part of the Merit-Based Incentive Payment System (MIPS). One of three performance categories to be scored for 2017 reporting, ACI will be worth 25% of your total MIPS Composite Performance Score. Non-physician eligible clinicians, hospital-based eligible clinicians, and non-patient facing eligible clinicians are considered ineligible for Advancing Care Information, and will have this performance category automatically re-weighted to zero.
Topics: MACRA & MIPS, Policy, ACI Performance Category
The MIPS Quality Performance Category is replacing PQRS reporting in 2017, folding it into the Merit-Based Incentive Payment System. The Quality portion will comprise 60% of an eligible clinician's MIPS Composite Performance Score for 2017. To calculate that score, there is significant math involved. This article will walk you though the calculations and logic used to determine your Quality score, but it is important to note that many data submission vendors will automatically give you a predictive calculation.
Topics: MACRA & MIPS, Policy, Quality Performance Category
In December we posted about a CMS announcement related to ICD-10 diagnosis and procedure code changes, and how this might affect payment adjustments in 2018. At the time CMS had not yet issued their addendum detailing specific code updates for measures being used in the Merit-Based Incentive Payment System (MIPS), but now that they have, here’s an update:
CMS and the National Library of Medicine (NLM) have published the addendum to the 2016 eCQM specifications which affects ICD-10 Clinical Modification (CM) and Procedure Coding System (PCS) value sets for 2017. Health Quality Measure Format (HQMF) specifications, value set object identifiers (OIDs), and measure version numbers for 2017 were not changed. The eCQM value set addendum for 2017 is published to the eCQM Library and the eCQI Resource Center. The NLM’s Value Set Authority Center also provides a complete list of revisions to the eCQM value sets.
Nearly 90 percent of healthcare organizations suffer data breaches according to the Ponemon Institute. [1] The level of data breaches is predicted to continue to grow.[4] What if there was a technology to better encrypt our health data, while also providing improved access to comprehensive health data for a patient? The quality of healthcare would rise, patient satisfaction would increase by leaps and bounds and costs would likely fall. Sound idylic?
Topics: Interoperability, Industry insights, Health IT
Medicare for all?
"We’re going to have insurance for everybody,” President-elect Donald Trump told the Washington Post in an interview over the weekend. "I don’t want single-payer. What I do want is to be able to take care of people.” So while we hear of Affordable Care Act (ACA, sometimes called Obamacare) repeal during the first 100 days of the administration, it sounds as if new programs must be quickly in the works to meet his mandate. “ The Congress can’t get cold feet because the people will not let that happen,” Trump continued, giving further emphasis to his push (and probably tweets) behind this initiative.
Topics: Policy
Satisfy the MIPS Improvement Activities Performance Category by Giving Feedback About MACRA!
With the introduction of MIPS reporting in 2017, and the launch of MIPSPRO, now is the time to be considering efficient ways of fulfilling MIPS requirements. CMS is conducting a study with the aim of better understanding practice's experiences quality reporting that will satisfy the Improvement Activities Performance Category of the Merit-Based Incentive Payment System (MIPS). Applications for this study are going to be accepted from January 1 - 31, 2017.
Topics: PRO Tips, MACRA & MIPS, Policy, IA Performance Category
As I sit in my office, I hear the Christmas decorations coming down. There is comfort in the known passing of the seasons and excitement at Healthmonix as we move into MIPS for 2017. Our new platform for MIPS is ready for launch. We are excited to see our efforts pay off for healthcare.
While the national election means that the Affordable Care Act will likely be changed, MACRA was passed with wide bipartisan support so will likely be staying in place. We at Healthmonix don’t believe the change in administration will affect the underlying efforts to transition to value-based care, either for MIPS or any other initiatives that we currently support. The triple aim (better care, lower cost, better patient experience) is still at the heart of what we do.
Topics: Healthmonix
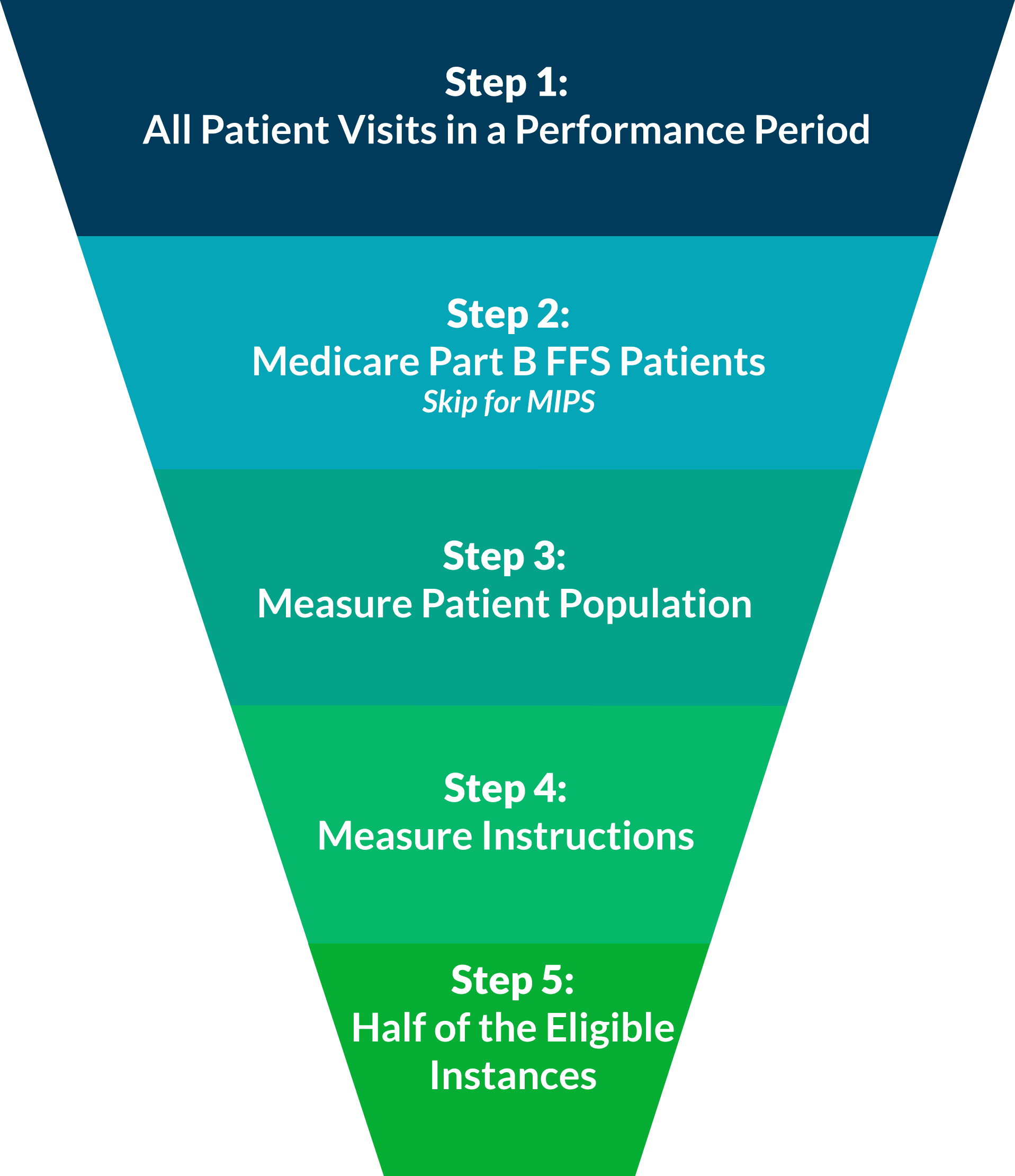
When reporting individual quality measures, whether it be for PQRS this year, or for one of the performance categories of MIPS next year, you are expected to report at least 50% of your eligible instances for each measure. In our experience, this concept can be confusing when practically applied. Luckily, it can be disambigusted in five easy steps!
Consider All Patient Visits for the Performance Period
A performance period for PQRS is based on a complete calendar year beginning on January 1 and ending on December 31.
For MIPS reporting, the performance period can range from a continuous 90-day period to the full calendar year.
Last night, a very surprising article was promoted, "CMS waves Physician Quality Reporting System penalties for 2017, 2018 after massive ICD-10 update clogs system." This post makes it seem as if only the Value-Based Modifier (VM) program penalties and incentives would still be in effect based on PQRS reporting done in 2015 and 2016. This is a dangerous misconception.