How Your MIPS Score Will Follow You (Even If You Leave Your Practice)
Topics: PRO Tips, MACRA & MIPS, Physician Compare, Policy
This One Major Disconnect May Devastate Hopes of MIPS Reporting Success
Considering that the CMS Quality Payment Program can generate payment adjustments of up to 22% of Medicare Part B FFS reimbursements, it’s no wonder that many providers and health systems hope to maximize these incentives. But navigating complex Medicare requirements can be near impossible without the right tools.
Topics: PRO Tips, MACRA & MIPS, EHR
With the first performance year of the Merit-based Incentive Payment System (MIPS) drawing to a close, you may have just started getting accustomed to how MIPS reporting works. Although the 2018 MACRA final rule introduced changes to how MIPS performance data should be captured for the upcoming performance year, it may be a relief to hear that largely the changes just build upon the existing 2017 regulations.
Topics: MACRA & MIPS, Policy, Quality Performance Category, ACI Performance Category, IA Performance Category, Cost Performance Category
Yesterday afternoon, CMS released the 2018 Final Rule for the MACRA Quality Payment Program. The rule finalized some changes we were expecting, and others that came as a surprise. The second year of the Quality Payment Program will be more advanced than the first, aiming to get clinicians ready for the even more intense requirements mandated by the MACRA legislation to be enacted in 2019.
Topics: MACRA & MIPS, Policy
The Second National MACRA MIPS/APM Summit is the leading forum on MACRA, MIPS, APMs, and other Value Based Payment Models. With no fee increases across-the-board for physicians from 2020-2025, value-based payment is going to become key for any health system's viability. Healthmonix was pleased to attend this summit and see MACRA policy and perspective in the making, with thought leaders in the medical, research, and business fields convening to break down MACRA and it's implementation now, as well as look towards the future of what MACRA can and should be.
We put together a brief list of takeaways from this event.
Topics: MACRA & MIPS, Industry insights, APMs
Value-based payment models aim to address rising healthcare costs, clinical inefficiency and duplication of services. To survive in an industry with increasing competition a solid understanding of the business case for implementing value based care is imperative.
The most notable value based care program currently is the MACRA Quality Payment Program, which provides the option to participate in MIPS or an advanced APM. If you’ve been keeping up with our blog posts recently you may already know that the deadline for the last MIPS performance period of the year is October 2nd, and that as long as you start collecting data by that date you will be able to report successfully.
Topics: MACRA & MIPS, VBC
To prosper in an industry challenged by constantly changing reform and increasing competition, healthcare organizations must continually increase their quality of care and become more efficient. Reporting MIPS in 2017 is a low-risk, high reward condition to stress-test your clinical workflows for optimized value-based program reporting.
Topics: MACRA & MIPS, Policy
CMS is worried about how few providers understand or are even aware of MACRA. As we near October 2nd, the deadline by which 400,000 eligible providers must start tracking data in order to avoid a financial penalty in 2019, CMS has found that around 40% of clinicians and even fewer nurse practitioners have a solid understanding of the requirements. Their concern is only supported by a recent Integra Connect survey which finds that most specialty physicians have not yet made the operational changes necessary to succeed in the new world of value based care.
Topics: MACRA & MIPS
Statistically, you aren’t sure how you’re supposed to comply with quality reporting requirements this year. As late as June 2017, the majority of providers were still unfamiliar or only somewhat familiar with MACRA; only 9 percent described themselves as “very familiar”. But unless you’re a part of that 9 percent, we highly recommend that you take some time ASAP to familiarize yourself with the requirements and to make a plan for the rest of the year. And as part of that plan, here are four reasons why we recommend that you select Improvement Activities for your practice today (yes, literally today):
Topics: PRO Tips, MACRA & MIPS, IA Performance Category
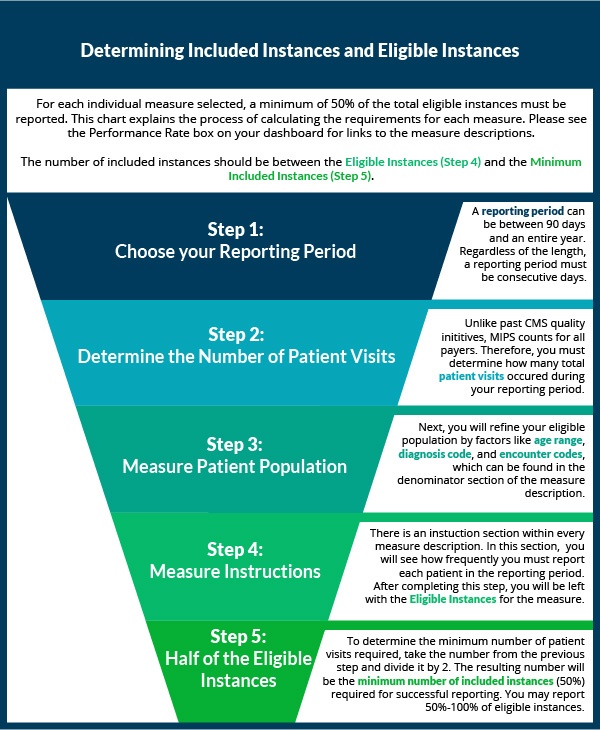
Data Completeness for MIPS Quality Measures [Infographic]
Over the last two weeks, we've shown you how to select quality measures. Now that you've decided which measures to collect data for, it's time to start reporting! If you have reported PQRS in the past, the process will be similar with a few major changes. Eligible clinicians who are new to reporting may want to first check out our article on the basics of quality measures prior to understanding how to completely report a quality measure.
Topics: MACRA & MIPS, Policy, Quality Performance Category