In our last post, we covered some of the basic questions you should be asking yourself when choosing quality measures to report under MIPS. In part two of this series, we go over a few more specific questions that can help guide you to picking the best measures for your practice.
Topics: MACRA & MIPS, Policy, Quality Performance Category
So you’re a MIPS-eligible clinician (if you’re not sure about your participation status, check out our post about how to find out), and you don’t want your practice to miss out on the reimbursement you know you deserve. But how should you decide which quality measures to actually report to CMS? How can you know if the measures you’re choosing will ultimately lead to reporting success, and is there a way to use those measures to not just fulfill the requirements but actually improve your practice? We’ve put together a two-part post to guide you through the most important factors to consider when deciding what might be best for you and your practice. First, the basics:
Topics: MACRA & MIPS, Policy, Quality Performance Category
 The shift from volume to value-based care can be frustrating, especially when the reasons behind such a significant change aren’t clear. But with an estimated 250,000 American deaths per year caused by medical errors, minimizing these errors is a noble and vital effort. Additionally, CMS is now raising the bar for healthcare providers with the assessment of quality metrics against benchmarks and peers. With that in mind, let’s break down the meaning of, and intentions behind, Quality Measures.
The shift from volume to value-based care can be frustrating, especially when the reasons behind such a significant change aren’t clear. But with an estimated 250,000 American deaths per year caused by medical errors, minimizing these errors is a noble and vital effort. Additionally, CMS is now raising the bar for healthcare providers with the assessment of quality metrics against benchmarks and peers. With that in mind, let’s break down the meaning of, and intentions behind, Quality Measures.
Topics: MACRA & MIPS, Policy, Quality Performance Category
Three Ways to Check Your MIPS Participation Eligibility Status
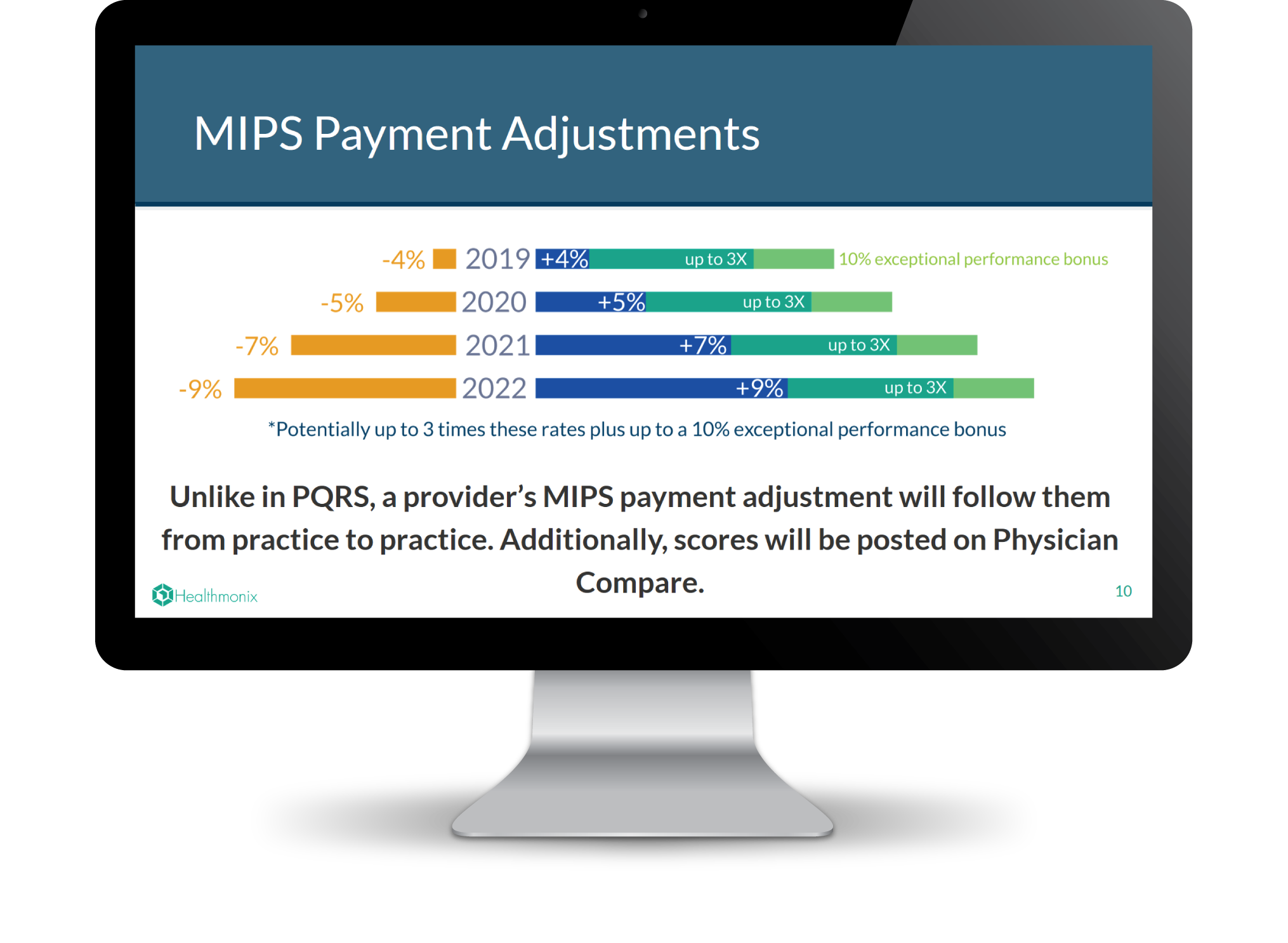
When we asked MIPS eligible clinicians about their experiences transitioning from PQRS this year, one of the biggest takeaways was that quality matters even more under MIPS than it did under PQRS. Clinicians who want to maximize their reimbursement would consequently be very smart to start reporting as early as possible, and to adjust performance to maximize quality, rather than waiting until the end of the year. If you’re not sure whether or not you are a MIPS-eligible clinician, take advantage of one of the following resources for determining your MIPS participation status as soon as possible so that you don’t get left behind.
Topics: PRO Tips, MACRA & MIPS, Eligibility
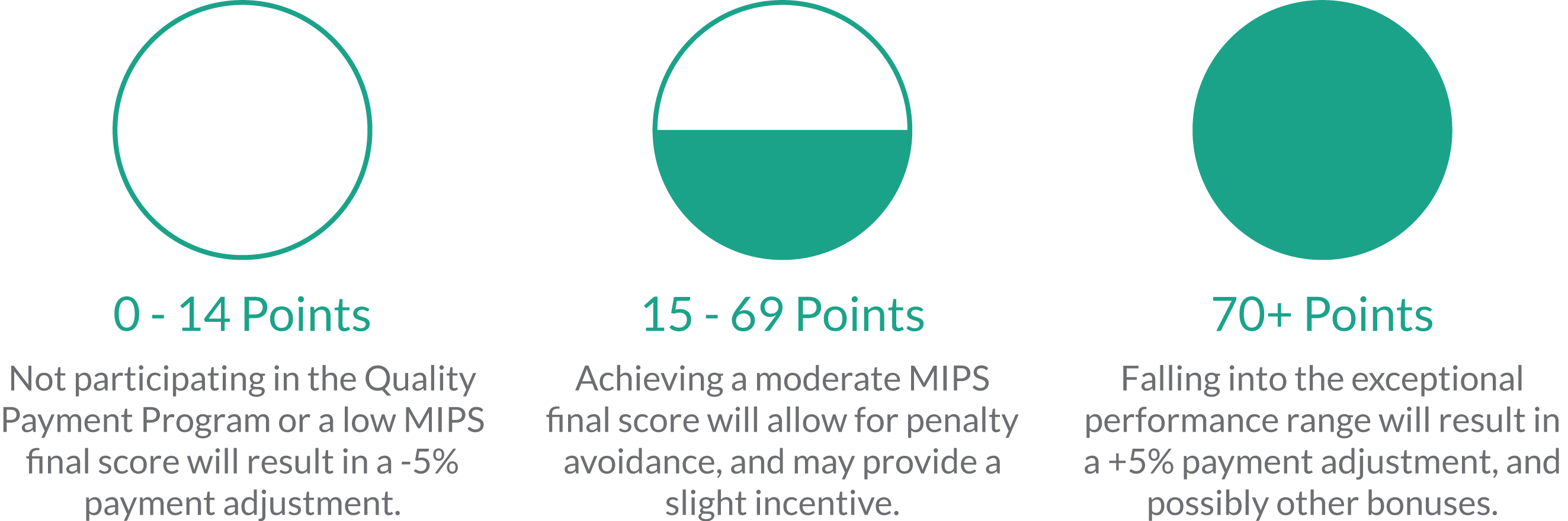
We are now in the seventh month of the new Merit-Based Incentive Payment System (MIPS), and the majority of MIPS-eligible clinicians still feel completely unprepared for success. With complicated and changing regulations, ensuring compliance can be a long and arduous process. Like most sizable goals, MIPS is best digested in small pieces, but it is hard to tell where to start sometimes. That is why we are going give you an order of operations to follow to ensure MIPS survival.
Topics: PRO Tips, MACRA & MIPS, CMS, Eligibility
Transparency is a vital aspect of the transition to quality care because it allows patients to make more informed healthcare choices. To this end, CMS has increased accessibility of physician information with the Physician Compare website, which publicly reports provider data including some quality measures. If you are a provider and want to assess or even optimize how you appear compared to your peers, you may have questions about how the Physician Compare website works and how to make sure it represents you accurately.
Topics: MACRA & MIPS, CMS, Physician Compare, Policy
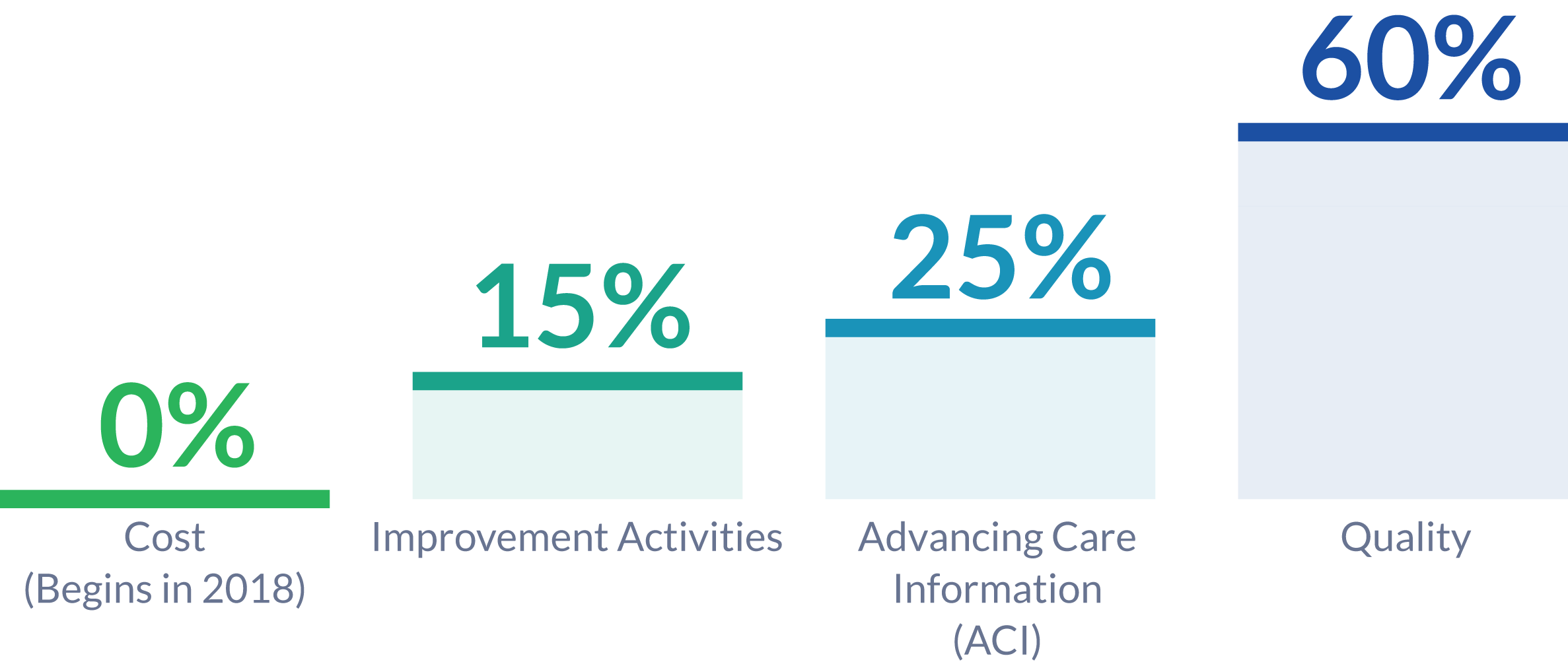
The 2018 Quality Payment Program proposed rule suggests significant changes to MIPS reporting. The changes proposed are aimed at easing the burden of reporting while increasing the meaningfulness of compliance. We have previously discussed new policies being introduced and changes compared to 2017 reporting. The 2018 proposed rule also suggests changes to the MIPS Performance Categories.
Topics: MACRA & MIPS, Policy
The 2018 MIPS Proposed Rule was just released by CMS, and it contains changes from the 2017 rule which providers may benefit from considering in relation to their reporting goals and strategies. In our last post we outlined various new proposals as well as new opportunities for bonus points in the MIPS final score. Here we clarify further changes from 2017, including updates on the low volume threshold, submission options, and the minimum performance period.
Topics: MACRA & MIPS, Policy
Yesterday afternoon, CMS posted CY 2018 Updates to the Quality Payment Program to the Federal Register, to be officially published at the end of this month. Many clinicians are still trying to wrap their heads around how to report MIPS in 2017. However, the release of the 2018 proposed rule is advantageous as aid deciding what to conquer in 2017, and which aspects of MIPS can be digested in the future. As the title suggests, this document also covers other Quality Payment Program tracks, like Advanced APMs. As the vast majority of healthcare providers are expected to be participating in MIPS for 2017 and 2018, we are just going to focus on the MIPS component of the proposed rule for now.
Topics: MACRA & MIPS, Policy
Maybe you’ve reported PQRS in the past and are already preparing to make the transition to MIPS this year. Or, maybe this year is the first time your practice plans to report. Either way, your method of reporting can help determine whether or not you achieve your quality and revenue goals, and the benefits and drawbacks of different methods must be weighed in relation to the unique needs of your practice. To give you a place to start, this post compares and contrasts some considerations related to two common submission mechanisms: EHR and Qualified MIPS Registry reporting.
Topics: PRO Tips, MACRA & MIPS, EHR, ROI