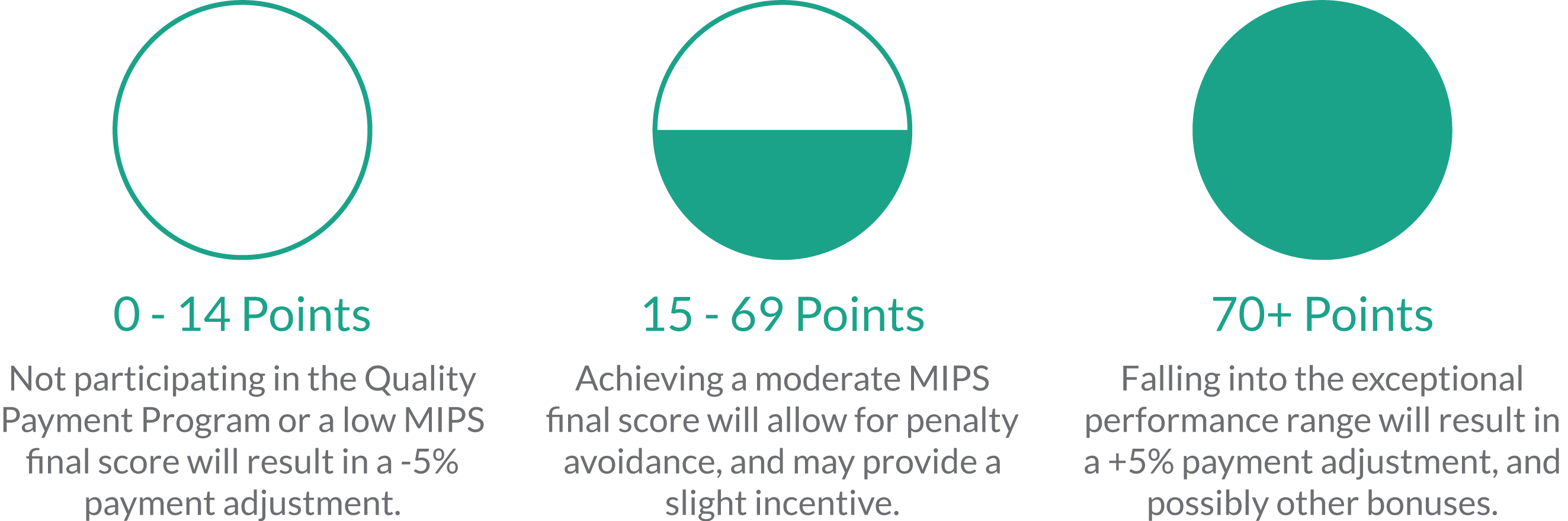
As we make our way through year two of the Quality Payment Program (QPP), it’s clearer than ever that simply reporting quality data is no longer enough. CMS penalties and incentives reach 5% in 2018, and in future years payment adjustments will continue to increase along with the percentage of patients you will be required to report on. Meeting quality standards and cutting costs are also increasingly important as measures are assessed against benchmarks and peers. Choosing the best reporting method for your practice is therefore an increasingly important step toward reporting efficiency and ultimately reporting success.
Topics: MACRA & MIPS, Policy, Administrative Burden
CMS Proposes Overhauling Meaningful Use: 4 Important Takeaways
On Tuesday April 24th, CMS released a proposed rule which essentially overhauls the Medicare and Medicaid Electronic Health Record Incentive Programs (also known as the “Meaningful Use” program). The proposed rule includes updates to Medicare payment policies and rates under the Inpatient Prospective Payment System (IPPS) and the Long-Term Care Hospital (LTCH) Prospective Payment System (PPS). Here are five things you should know about the proposed changes:
Topics: CMS, Interoperability, Policy, ACI Performance Category, PI Performance Category
Topics: MACRA & MIPS, Policy
In year two of MIPS and beyond, CMS is including an Improvement score for Quality and Cost measures. This week we take a deep dive into what this score entails, as well as what you need to know to keep yours ahead of the curve.
Topics: MACRA & MIPS, Policy, Quality Performance Category, Cost Performance Category
Depending on your performance and your desire to maximize your reimbursement in 2019 (who doesn’t want more revenue?), there are a number of options available in final submission of your MIPS data to CMS. All of these choices can seem overwhelming, but Healthmonix is here to help! Read on to find out what choices you'll face and how to make the best ones for your practice.
Topics: PRO Tips, MACRA & MIPS, Policy
How Your MIPS Score Will Follow You (Even If You Leave Your Practice)
Topics: PRO Tips, MACRA & MIPS, Physician Compare, Policy
What The Individual Mandate Repeal Means For Your Premiums
Today the president signed the Tax Cuts and Jobs Act, a bill which will have far-reaching implications for tax reform, into law. But the legislation may also affect the health insurance market through its elimination of the ACA individual mandate. In this week’s blog we look in-depth at what the repeal of the individual mandate entails, as well as its potential effect on the insurance marketplace.
Topics: Policy
With the first performance year of the Merit-based Incentive Payment System (MIPS) drawing to a close, you may have just started getting accustomed to how MIPS reporting works. Although the 2018 MACRA final rule introduced changes to how MIPS performance data should be captured for the upcoming performance year, it may be a relief to hear that largely the changes just build upon the existing 2017 regulations.
Topics: MACRA & MIPS, Policy, Quality Performance Category, ACI Performance Category, IA Performance Category, Cost Performance Category
Yesterday afternoon, CMS released the 2018 Final Rule for the MACRA Quality Payment Program. The rule finalized some changes we were expecting, and others that came as a surprise. The second year of the Quality Payment Program will be more advanced than the first, aiming to get clinicians ready for the even more intense requirements mandated by the MACRA legislation to be enacted in 2019.
Topics: MACRA & MIPS, Policy
To prosper in an industry challenged by constantly changing reform and increasing competition, healthcare organizations must continually increase their quality of care and become more efficient. Reporting MIPS in 2017 is a low-risk, high reward condition to stress-test your clinical workflows for optimized value-based program reporting.
Topics: MACRA & MIPS, Policy