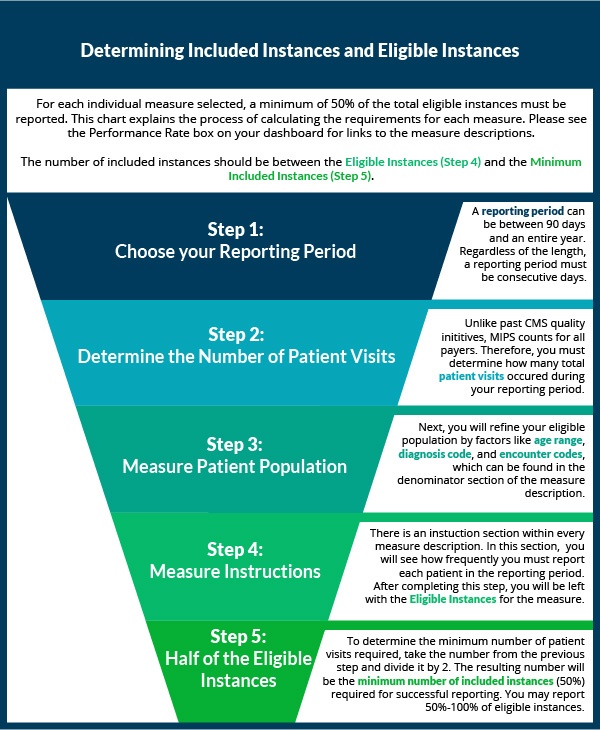
Over the last two weeks, we've shown you how to select quality measures. Now that you've decided which measures to collect data for, it's time to start reporting! If you have reported PQRS in the past, the process will be similar with a few major changes. Eligible clinicians who are new to reporting may want to first check out our article on the basics of quality measures prior to understanding how to completely report a quality measure.
Data Completeness for MIPS Quality Measures [Infographic]
Topics: MACRA & MIPS, Policy, Quality Performance Category
In our last post, we covered some of the basic questions you should be asking yourself when choosing quality measures to report under MIPS. In part two of this series, we go over a few more specific questions that can help guide you to picking the best measures for your practice.
Topics: MACRA & MIPS, Policy, Quality Performance Category
So you’re a MIPS-eligible clinician (if you’re not sure about your participation status, check out our post about how to find out), and you don’t want your practice to miss out on the reimbursement you know you deserve. But how should you decide which quality measures to actually report to CMS? How can you know if the measures you’re choosing will ultimately lead to reporting success, and is there a way to use those measures to not just fulfill the requirements but actually improve your practice? We’ve put together a two-part post to guide you through the most important factors to consider when deciding what might be best for you and your practice. First, the basics:
Topics: MACRA & MIPS, Policy, Quality Performance Category
 The shift from volume to value-based care can be frustrating, especially when the reasons behind such a significant change aren’t clear. But with an estimated 250,000 American deaths per year caused by medical errors, minimizing these errors is a noble and vital effort. Additionally, CMS is now raising the bar for healthcare providers with the assessment of quality metrics against benchmarks and peers. With that in mind, let’s break down the meaning of, and intentions behind, Quality Measures.
The shift from volume to value-based care can be frustrating, especially when the reasons behind such a significant change aren’t clear. But with an estimated 250,000 American deaths per year caused by medical errors, minimizing these errors is a noble and vital effort. Additionally, CMS is now raising the bar for healthcare providers with the assessment of quality metrics against benchmarks and peers. With that in mind, let’s break down the meaning of, and intentions behind, Quality Measures.
Topics: MACRA & MIPS, Policy, Quality Performance Category
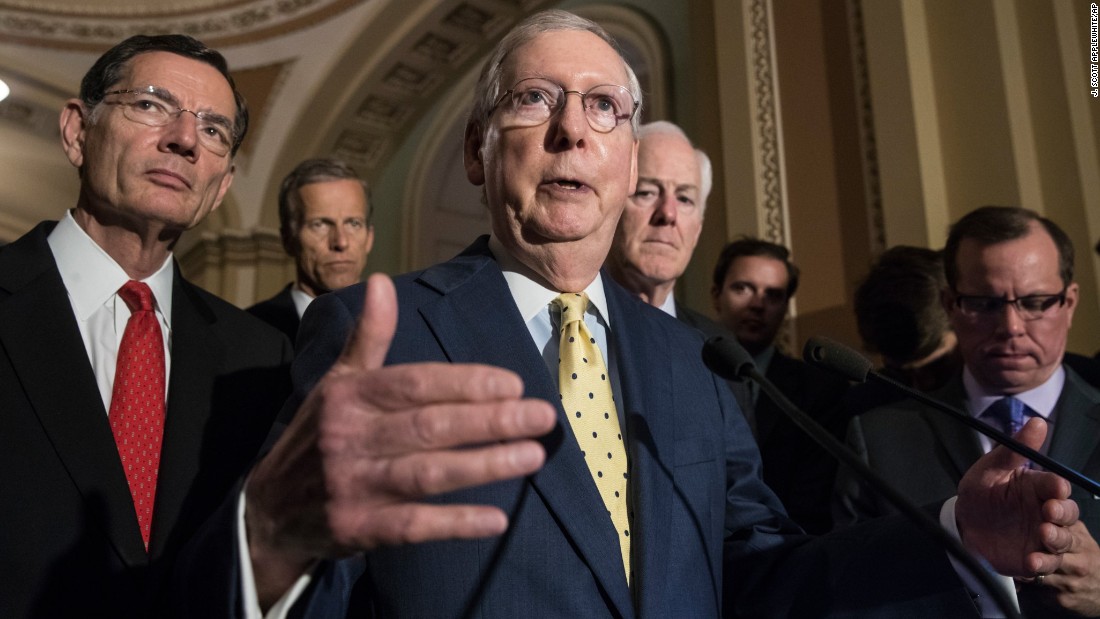
On Monday night this week, in the wake of news that there might not be enough votes to pass the updated Senate version of the AHCA, Senate Majority Leader Mitch McConnell (R-KY) announced a plan to vote for legislation that would repeal most of Obamacare without immediately putting an alternative in place. The alternative plan would instead be developed over the course of the next two years.
Topics: Policy
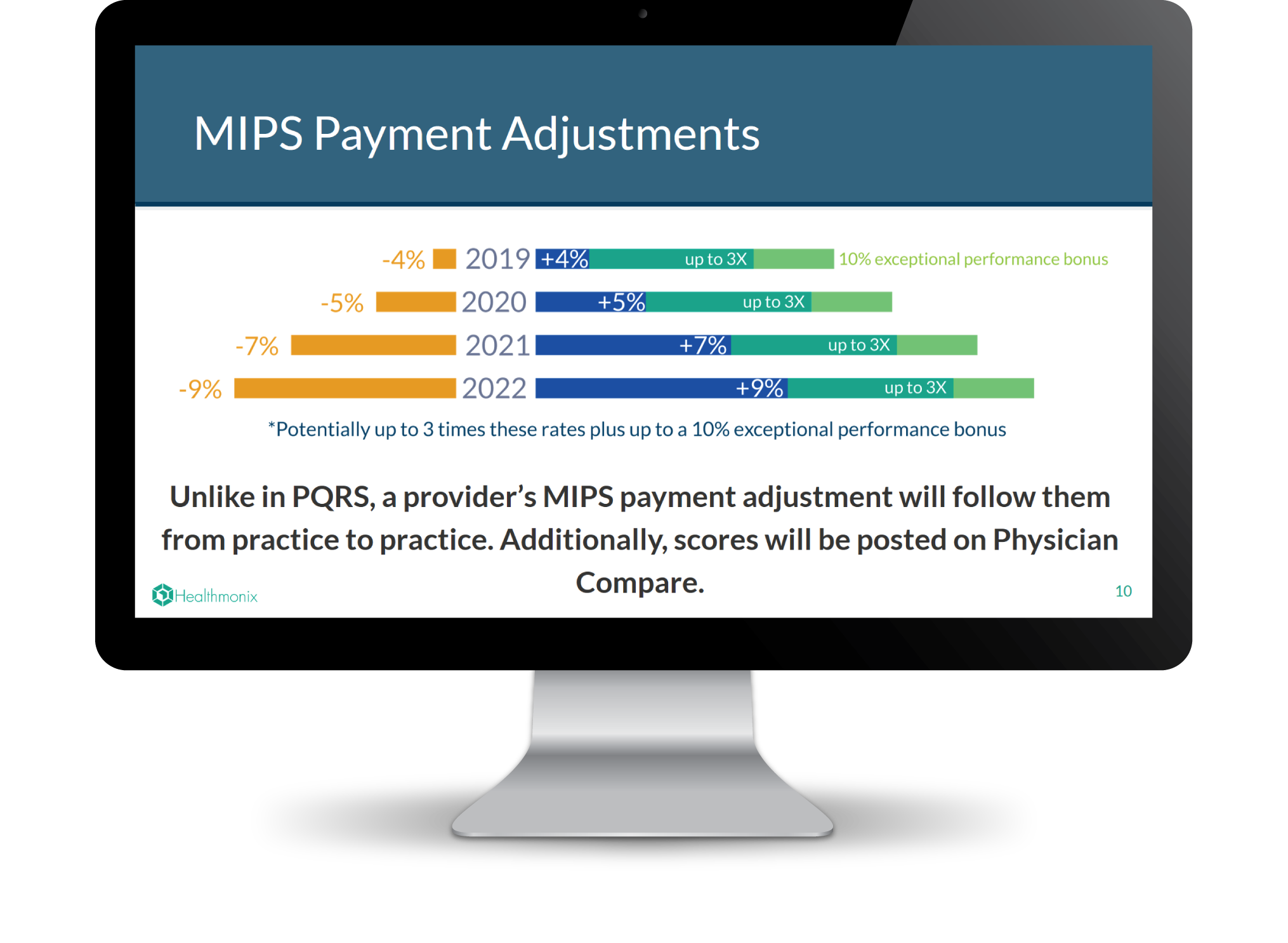
Transparency is a vital aspect of the transition to quality care because it allows patients to make more informed healthcare choices. To this end, CMS has increased accessibility of physician information with the Physician Compare website, which publicly reports provider data including some quality measures. If you are a provider and want to assess or even optimize how you appear compared to your peers, you may have questions about how the Physician Compare website works and how to make sure it represents you accurately.
Topics: MACRA & MIPS, CMS, Physician Compare, Policy
The American Health Care Act (AHCA), also known as Trumpcare, was narrowly passed through the House of Representatives on Thursday May 4th. On Thursday June 22nd, after a secretive seven-week revision process led by Majority Leader Mitch McConnell, a draft of the Senate version of the bill has been released. Following is a comparison of some of the important changes between the ACA (Obamacare) and both versions of the AHCA.
Topics: Policy
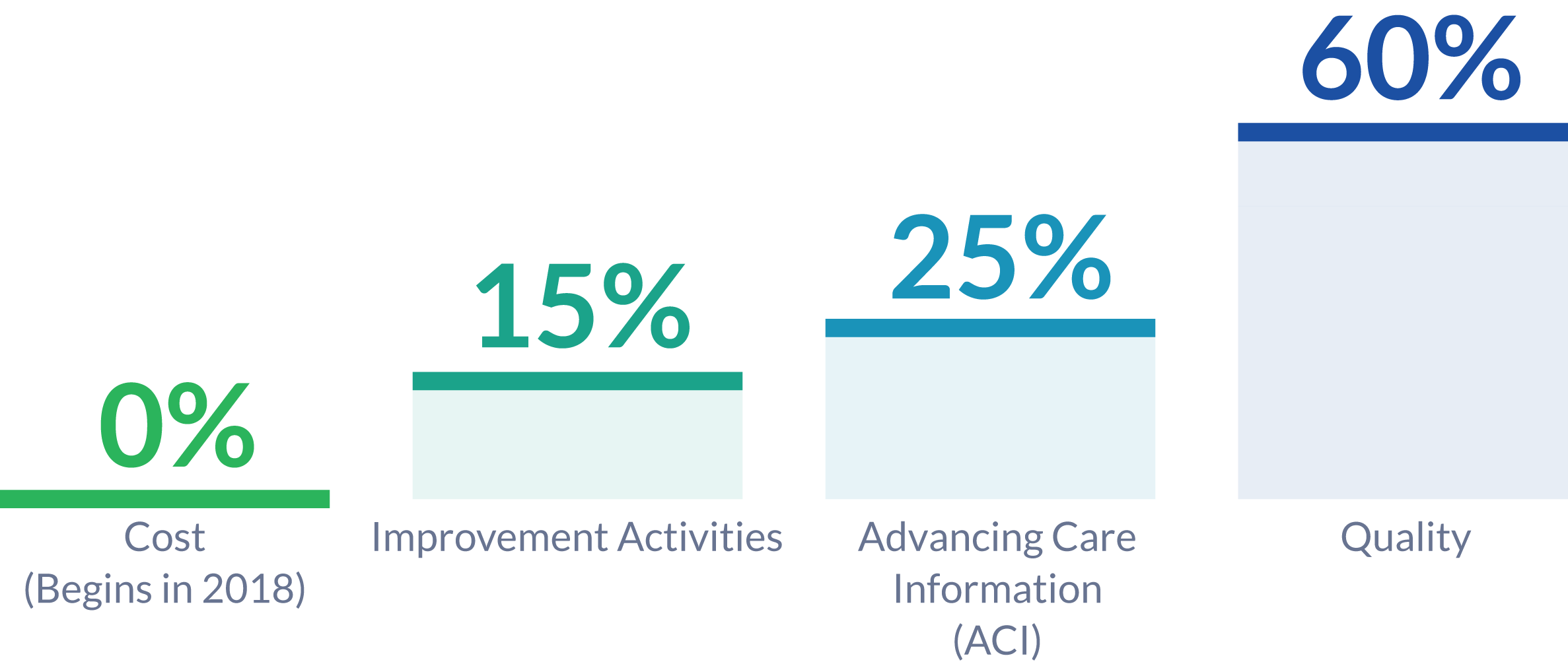
The 2018 Quality Payment Program proposed rule suggests significant changes to MIPS reporting. The changes proposed are aimed at easing the burden of reporting while increasing the meaningfulness of compliance. We have previously discussed new policies being introduced and changes compared to 2017 reporting. The 2018 proposed rule also suggests changes to the MIPS Performance Categories.
Topics: MACRA & MIPS, Policy
The 2018 MIPS Proposed Rule was just released by CMS, and it contains changes from the 2017 rule which providers may benefit from considering in relation to their reporting goals and strategies. In our last post we outlined various new proposals as well as new opportunities for bonus points in the MIPS final score. Here we clarify further changes from 2017, including updates on the low volume threshold, submission options, and the minimum performance period.
Topics: MACRA & MIPS, Policy
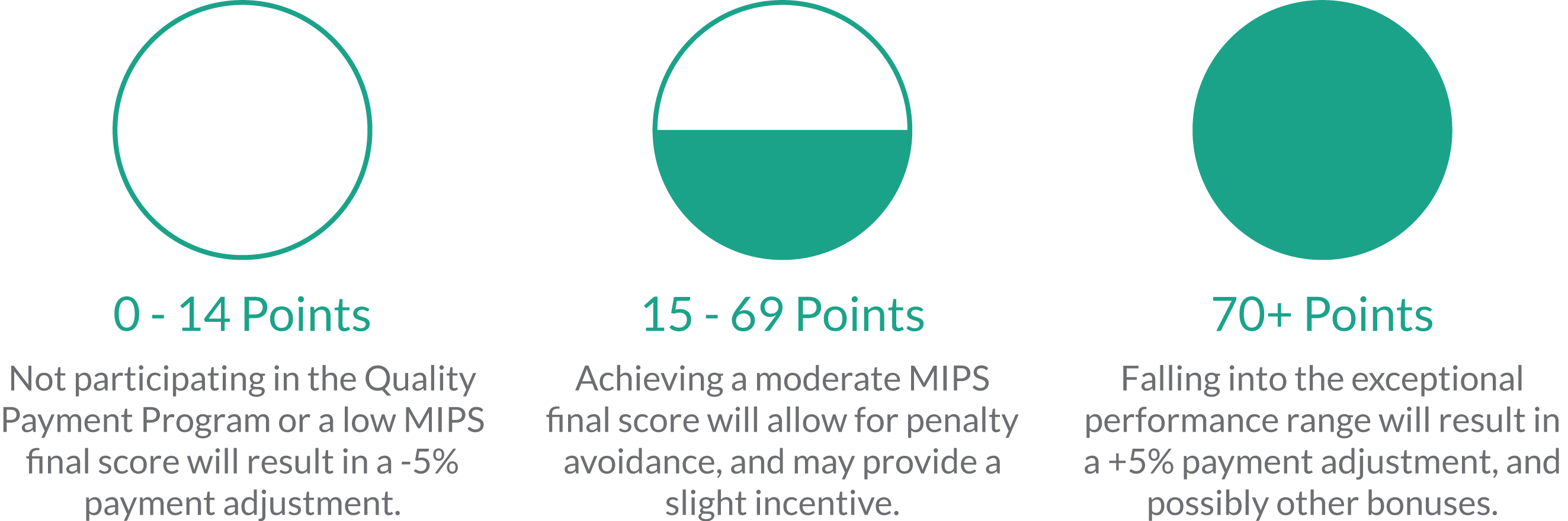
Yesterday afternoon, CMS posted CY 2018 Updates to the Quality Payment Program to the Federal Register, to be officially published at the end of this month. Many clinicians are still trying to wrap their heads around how to report MIPS in 2017. However, the release of the 2018 proposed rule is advantageous as aid deciding what to conquer in 2017, and which aspects of MIPS can be digested in the future. As the title suggests, this document also covers other Quality Payment Program tracks, like Advanced APMs. As the vast majority of healthcare providers are expected to be participating in MIPS for 2017 and 2018, we are just going to focus on the MIPS component of the proposed rule for now.
Topics: MACRA & MIPS, Policy