Apply to help CMS in its new study, running from April 2018 through March 2019, and make your voice heard.
CMS is looking for groups and individuals that are eligilbe for MIPS to help study the burden that the MIPS program, particularly the Quality component, place on eligible clinicians. In return, successful participants will receive full credit for the Improvement Activity component of MIPS this year (2018).
Read More
Topics:
MACRA & MIPS,
CMS,
Quality Performance Category,
Administrative Burden
In late October, CMS launched a new initiative, Patients Over Paperwork, targeted to reduce unproductive regulatory burdens on health care providers and increase efficiency. CMS Administrator Seema Verma announced the initiative during a stakeholder meeting with more than 30 industry groups.
The initiative is potentially wide reaching, affecting a broad range of regulations surrounding practices such as prior authorizations, documentation of evaluation and management codes, OIG audits, and EHR requirements.
According to Verma, this has already touched the QPP final rule for 2018. As an outcome of this initiative, the QPP final rule includes policies that exclude individual MIPS eligible clinicians with less than or equal to $90,000 in Part B allowed charges or less than or equal to 200 Part B beneficiaries.
Read More
Topics:
CMS
On October 30, CMS Administrator Seema Verma announced the Meaningful Measures initiative, which is intended to streamline quality reporting. This initiative is meant to address common criticisms of today’s performance measures, including their excessive focus on evaluating processes and the lack of alignment between programs. According to Verma, “Meaningful Measures will involve only assessing those core issues that are the most vital to providing high-quality care and improving patient outcomes.”
Read More
Topics:
CMS
We are now in the seventh month of the new Merit-Based Incentive Payment System (MIPS), and the majority of MIPS-eligible clinicians still feel completely unprepared for success. With complicated and changing regulations, ensuring compliance can be a long and arduous process. Like most sizable goals, MIPS is best digested in small pieces, but it is hard to tell where to start sometimes. That is why we are going give you an order of operations to follow to ensure MIPS survival.
Read More
Topics:
PRO Tips,
MACRA & MIPS,
CMS,
Eligibility
Transparency is a vital aspect of the transition to quality care because it allows patients to make more informed healthcare choices. To this end, CMS has increased accessibility of physician information with the Physician Compare website, which publicly reports provider data including some quality measures. If you are a provider and want to assess or even optimize how you appear compared to your peers, you may have questions about how the Physician Compare website works and how to make sure it represents you accurately.
Read More
Topics:
MACRA & MIPS,
CMS,
Physician Compare,
Policy
The first performance year of the Merit-based Incentive Payment System (MIPS) is well underway. One of the most marked differences between MIPS and previous CMS initiatives is the quality of educational resources available to eligible clinicians. However, wading through all the different documents can be confusing if you are just starting out. This article will walk you through the available resources for each step of your MIPS educational journey.
Read More
Topics:
MACRA & MIPS,
CMS
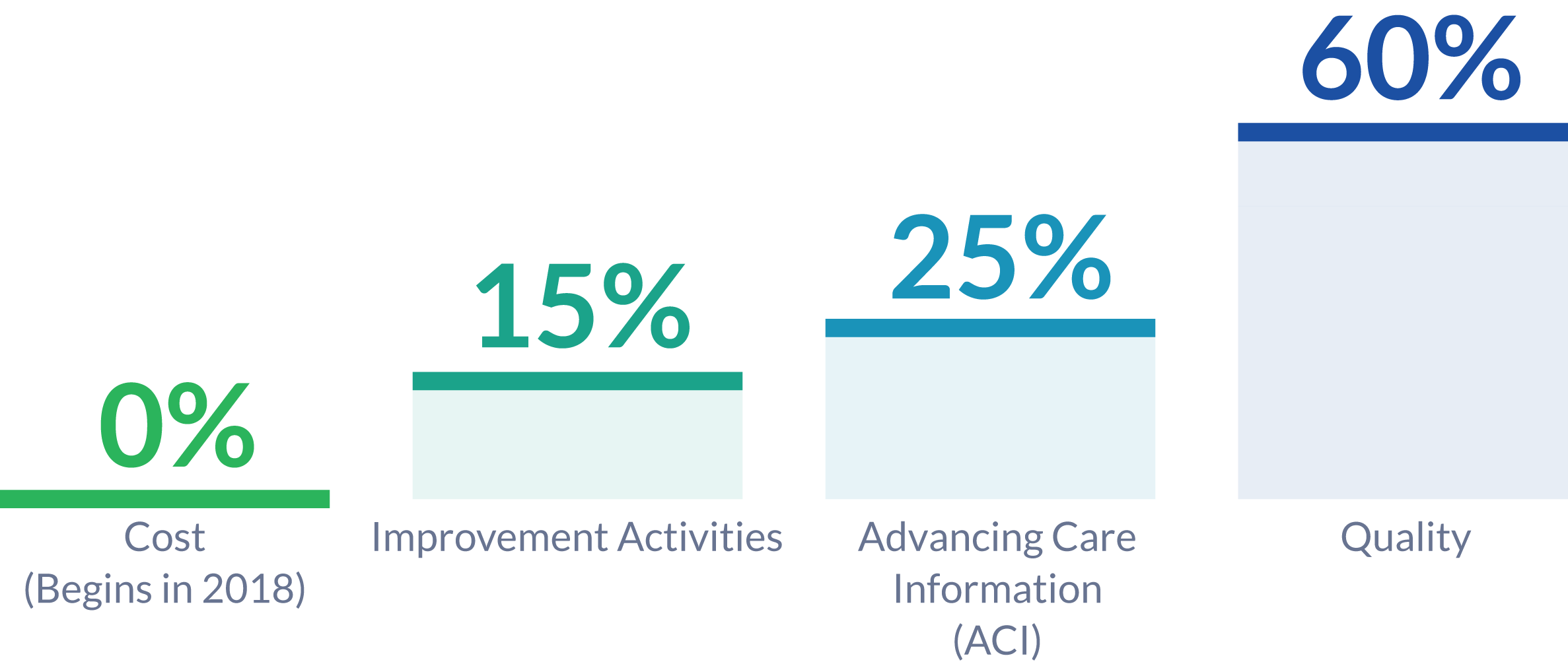
Malvern, PA – March 16, 2017 – Healthmonix was first-to-market with an all-inclusive solution for MIPS reporting, MIPSPROTM. This Qualified MIPS Registry is an end-to-end reporting solution, supporting the Quality, Advancing Care Information, and Improvement Activity Performance Categories of the Merit-Based Incentive Payment System (MIPS). The MIPSPRO engine also provides sophisticated real-time performance analytics, critical to competing for top MIPS incentives and improving patient outcomes.
Read More
Topics:
MACRA & MIPS,
CMS,
Healthmonix
Compared to the commotion surrounding other Trump administration nominees, Seema Verma's confirmation hearing passed by last Thursday with relatively little controversy. Despite the low level of coverage, understanding the contents of this hearing is imperative for predicting the next few years in American health care. As the Administrator for the Centers for Medicare and Medicaid Services (CMS), Seema Verma will shape the future of health care for 34% of Americans. [1]
Read More
Topics:
MACRA & MIPS,
CMS
Early on the morning of February 10th, the Senate approved the nomination of now-former Rep. Tom Price to be the Secretary of Health and Human Services. While some say his chief priority is “dismantling of the Affordable Care Act” (Sen. Maria Cantwell of Washington), the tasks that will be put in front of him also include five major health IT initiatives: appointments to ONC and other agencies, the future of MACRA and Meaningful Use, the enforcement of interoperability, telemedicine, and cybersecurity.
Read More
Topics:
MACRA & MIPS,
CMS,
Industry insights
In December we posted about a CMS announcement related to ICD-10 diagnosis and procedure code changes, and how this might affect payment adjustments in 2018. At the time CMS had not yet issued their addendum detailing specific code updates for measures being used in the Merit-Based Incentive Payment System (MIPS), but now that they have, here’s an update:
CMS and the National Library of Medicine (NLM) have published the addendum to the 2016 eCQM specifications which affects ICD-10 Clinical Modification (CM) and Procedure Coding System (PCS) value sets for 2017. Health Quality Measure Format (HQMF) specifications, value set object identifiers (OIDs), and measure version numbers for 2017 were not changed. The eCQM value set addendum for 2017 is published to the eCQM Library and the eCQI Resource Center. The NLM’s Value Set Authority Center also provides a complete list of revisions to the eCQM value sets.
Read More
Topics:
PQRS,
CMS,
Policy