This week, house Republicans introduced the long-anticipated Obamacare replacement plan. This plan, called the American Healthcare Act (AHCA), has received a high level of criticism already from a surprising mix of people. Although it certainly is too soon to tell, it seems as if the bill will likely not pass before significant edits are made.
Christina Zink
Recent Posts
Compared to the commotion surrounding other Trump administration nominees, Seema Verma's confirmation hearing passed by last Thursday with relatively little controversy. Despite the low level of coverage, understanding the contents of this hearing is imperative for predicting the next few years in American health care. As the Administrator for the Centers for Medicare and Medicaid Services (CMS), Seema Verma will shape the future of health care for 34% of Americans. [1]
Topics: MACRA & MIPS, CMS
Scoring the MIPS Advancing Care Information (ACI) Performance Category in 2017
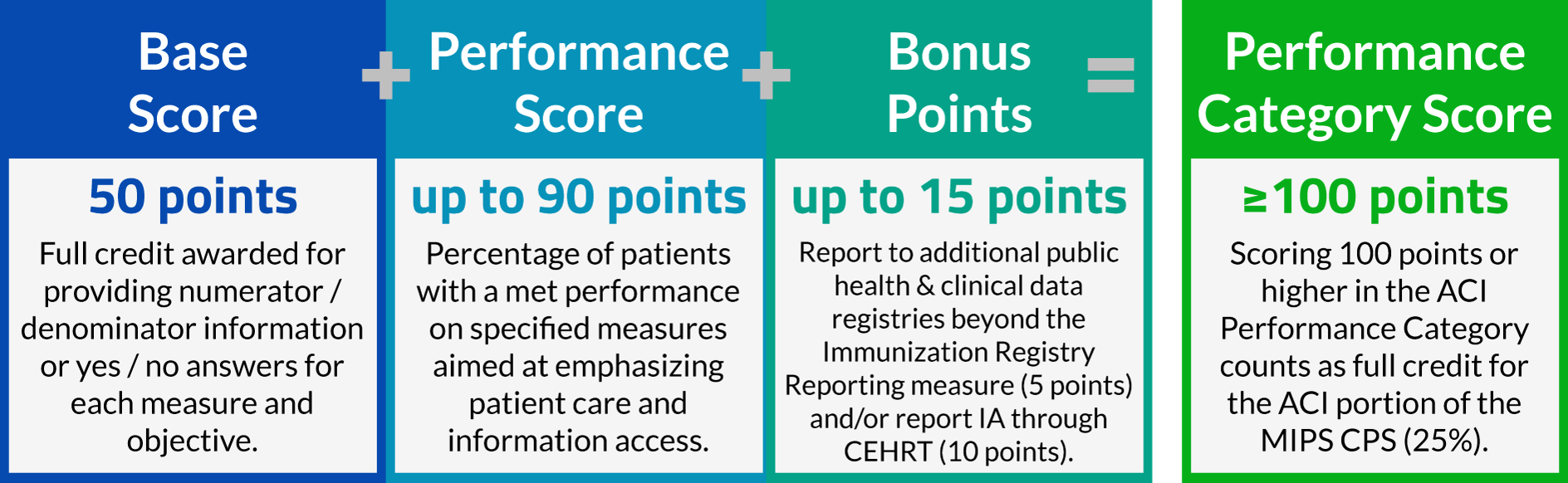
The Advancing Care Information Performance Category will be replacing the EHR Incentive Program (colloquially known as Meaningful Use) for 2017 performance year, as a part of the Merit-Based Incentive Payment System (MIPS). One of three performance categories to be scored for 2017 reporting, ACI will be worth 25% of your total MIPS Composite Performance Score. Non-physician eligible clinicians, hospital-based eligible clinicians, and non-patient facing eligible clinicians are considered ineligible for Advancing Care Information, and will have this performance category automatically re-weighted to zero.
Topics: MACRA & MIPS, Policy, ACI Performance Category
Satisfy the MIPS Improvement Activities Performance Category by Giving Feedback About MACRA!
With the introduction of MIPS reporting in 2017, and the launch of MIPSPRO, now is the time to be considering efficient ways of fulfilling MIPS requirements. CMS is conducting a study with the aim of better understanding practice's experiences quality reporting that will satisfy the Improvement Activities Performance Category of the Merit-Based Incentive Payment System (MIPS). Applications for this study are going to be accepted from January 1 - 31, 2017.
Topics: PRO Tips, MACRA & MIPS, Policy, IA Performance Category
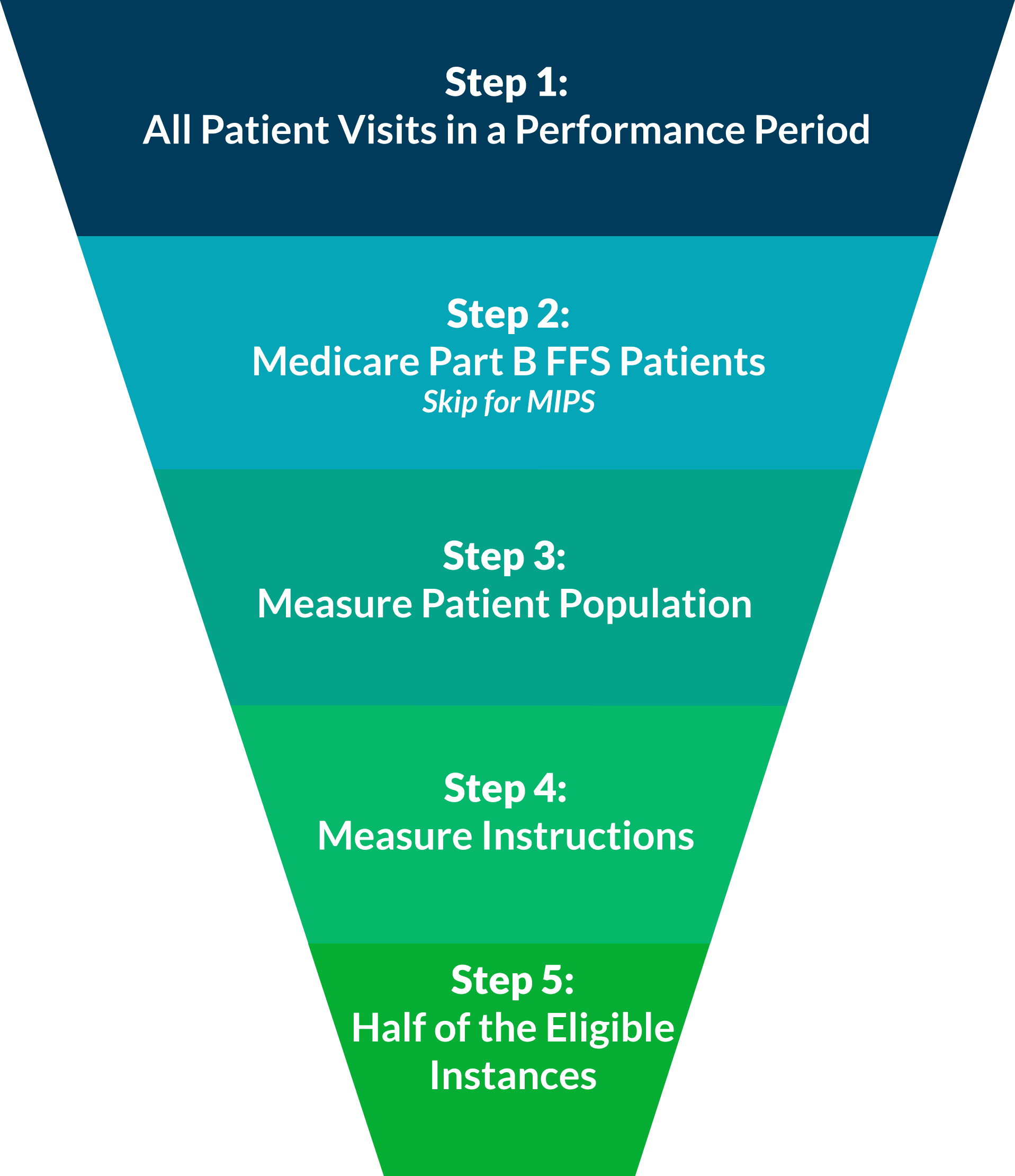
When reporting individual quality measures, whether it be for PQRS this year, or for one of the performance categories of MIPS next year, you are expected to report at least 50% of your eligible instances for each measure. In our experience, this concept can be confusing when practically applied. Luckily, it can be disambigusted in five easy steps!
Consider All Patient Visits for the Performance Period
A performance period for PQRS is based on a complete calendar year beginning on January 1 and ending on December 31.
For MIPS reporting, the performance period can range from a continuous 90-day period to the full calendar year.
Last night, a very surprising article was promoted, "CMS waves Physician Quality Reporting System penalties for 2017, 2018 after massive ICD-10 update clogs system." This post makes it seem as if only the Value-Based Modifier (VM) program penalties and incentives would still be in effect based on PQRS reporting done in 2015 and 2016. This is a dangerous misconception.
Once you've selected how you will report, the next step is to determine what you will report. This is called your reporting method. You have two options: reporting a measures group or reporting individual measures.
Last week, we discussed the first step to reporting PQRS in 2016, selecting a submission mechanism. To briefly recap, there are three submission mechanisms that are viable for practices starting to report at this point in the year: Registry, EHR, and QCDR. Of these three options, Registry reporting has the highest rate of success and ease of submission.
Reporting PQRS in 2016 is just as important as ever, with up to 6% of your Medicare Part B reimbursements on the line in 2018. According to the latest PQRS experience report[1], about 66% of eligible providers are participating in PQRS. Of these participating providers, 68% are still reporting using the claims-based reporting mechanism, which has an abysmal 40% success rate in avoiding the PQRS penalty. Just taking these numbers into account, this takes us up to at least 61% of PQRS eligible providers not avoiding the PQRS penalty.
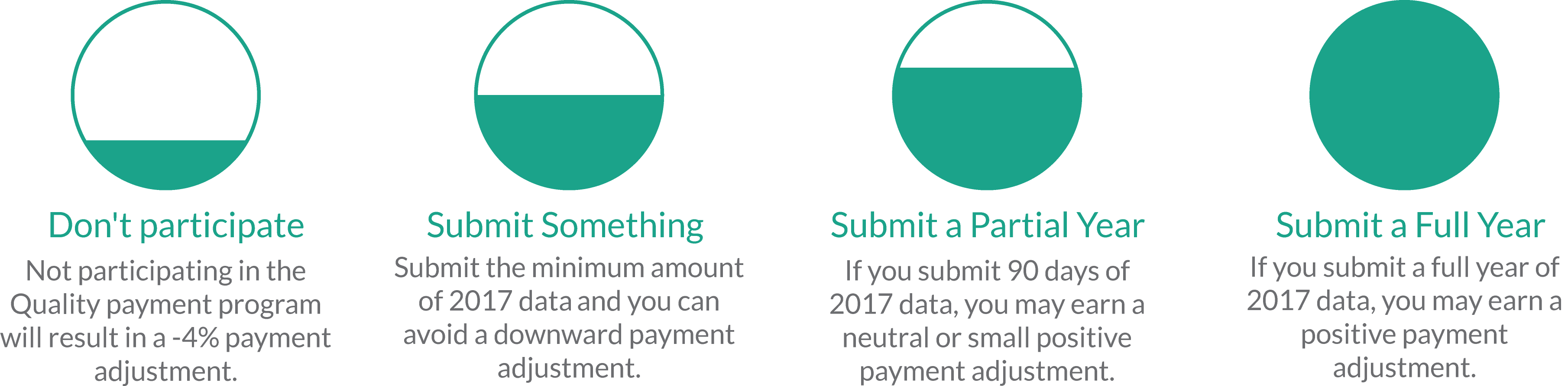
Thanksgiving is almost here! For me, this means reflecting on the things in my life that I am thankful for. Along with the tasty food I am about to consume with my loved ones, this year I am grateful for the MACRA Quality Payment Program. This may sound perplexing to you, as the MACRA Quality Payment Program has been causing a lot of alarm in the healthcare industry since the Notice of Proposed Rule Making (NPRM). However, with the release of the final rule came many provisions that I believe will improve the ease of reporting for clinicians while continuing to improve the quality of care for patients.
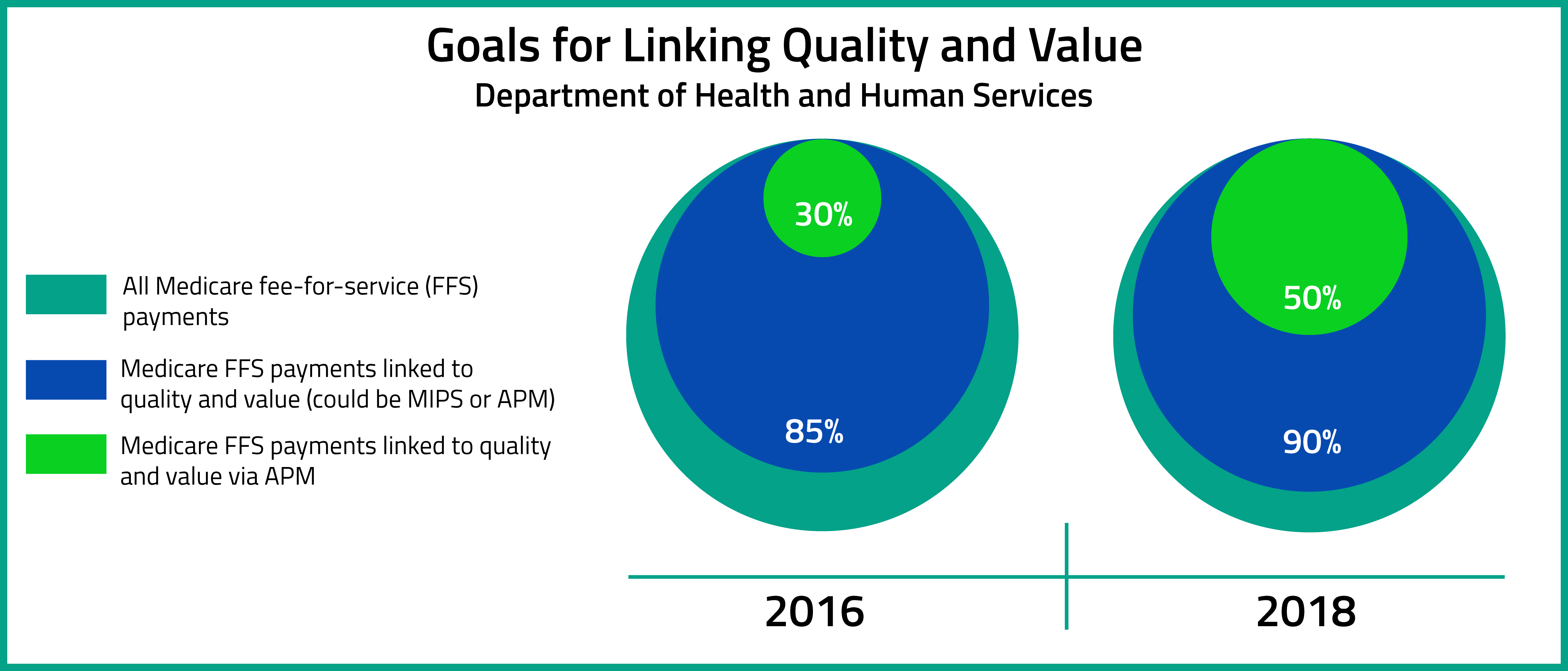
To briefly refresh before jumping in, the MACRA Quality Payment Program is split into two paths: the Merit-Based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (Advanced APMs). MIPS streamlines pre-existing CMS quality initiatives (like PQRS and Meaningful Use), while Advanced APMs are designed to encourage innovative value-based payment models.
Topics: MACRA & MIPS, Interoperability, Industry insights
Top Three Questions about Advanced Alternative Payment Model (APM) Participation
On October 14, 2016, the Department of Health and Human Services release the MACRA Quality Payment Program Final Rule. According to the Executive Summary of the Final Rule, the aims of the Quality Payment Program are to : "(1) support care improvement by focusing on better outcomes for patients, decreased provider burden, and preservation of independent clinical practice; (2) promote adoption of Alternative Payment Models that align incentives across healthcare stakeholders; and (3) advance existing efforts of Delivery System Reform, including ensuring a smooth transition to a new system that promotes high-quality, efficient care through unification of CMS legacy programs."[1]
Topics: MACRA & MIPS, Policy, Eligibility, APMs