In a new proposal titled “Pathways to Success,” the Centers for Medicare & Medicaid Services (CMS) has laid out a modified set of participation options for ACOs (accountable care organizations) in the Medicare Shared Savings Program (MSSP). The proposed participation options would no longer include an “upside-only” risk model; instead, ACOs would be required to select one of two tracks, both of which ultimately include some downside risk.
Primaris Partners with Healthmonix to Provide MIPS and ACO Reporting Solutions
Primaris and Healthmonix have joined forces to help healthcare providers meet and exceed new regulations that tie the quality of patient care to the payment for that care.
Topics: ACO, Healthmonix, APMs
Nail Your 2018 QPP Reporting with the Help of our MACRA Specialists
Over the past year, we tracked over 11 million patients with over 2 BILLION quality actions in MIPS reporting alone! We are already back to work and developing some really cool new analytic solutions to help our clients optimize their Quality outcomes.
Topics: MACRA & MIPS, Healthmonix, APMs
The Second National MACRA MIPS/APM Summit is the leading forum on MACRA, MIPS, APMs, and other Value Based Payment Models. With no fee increases across-the-board for physicians from 2020-2025, value-based payment is going to become key for any health system's viability. Healthmonix was pleased to attend this summit and see MACRA policy and perspective in the making, with thought leaders in the medical, research, and business fields convening to break down MACRA and it's implementation now, as well as look towards the future of what MACRA can and should be.
We put together a brief list of takeaways from this event.
Topics: MACRA & MIPS, Industry insights, APMs
Top Three Questions about Advanced Alternative Payment Model (APM) Participation
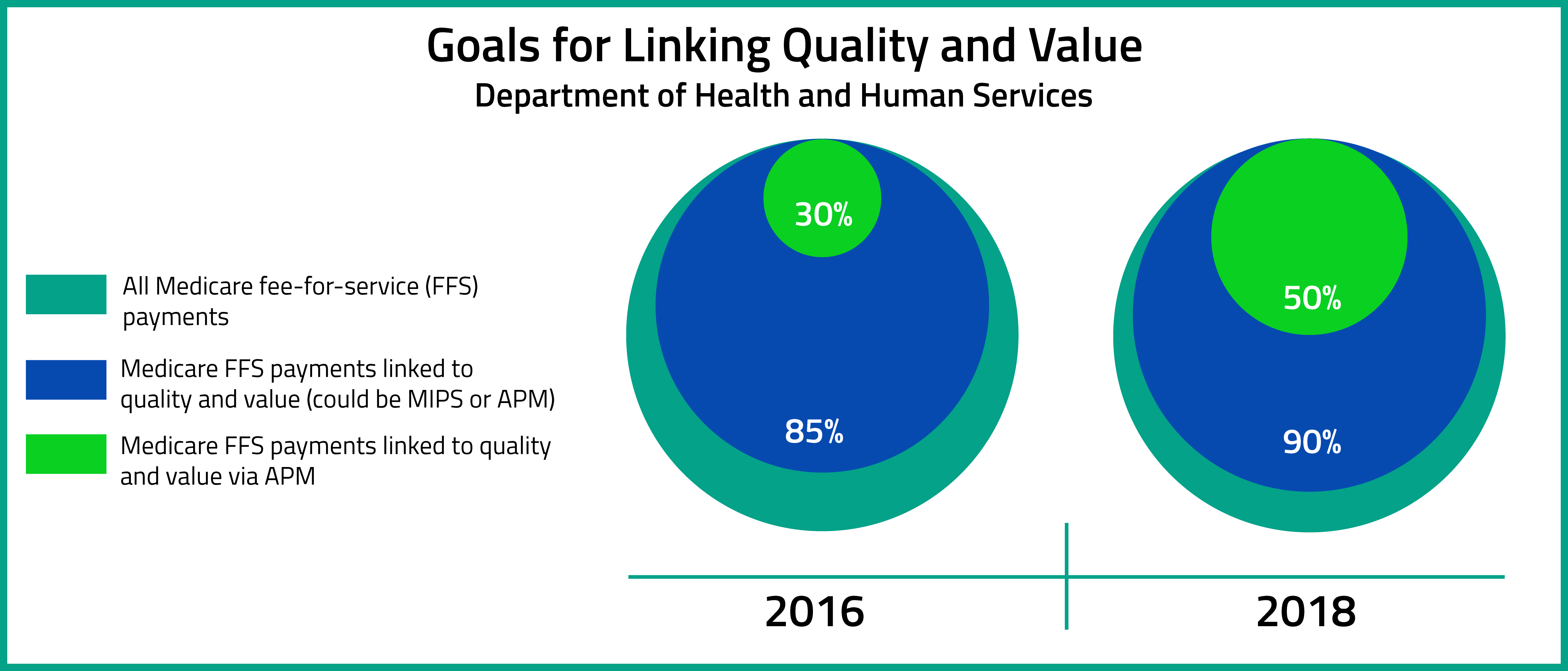
On October 14, 2016, the Department of Health and Human Services release the MACRA Quality Payment Program Final Rule. According to the Executive Summary of the Final Rule, the aims of the Quality Payment Program are to : "(1) support care improvement by focusing on better outcomes for patients, decreased provider burden, and preservation of independent clinical practice; (2) promote adoption of Alternative Payment Models that align incentives across healthcare stakeholders; and (3) advance existing efforts of Delivery System Reform, including ensuring a smooth transition to a new system that promotes high-quality, efficient care through unification of CMS legacy programs."[1]
Topics: MACRA & MIPS, Policy, Eligibility, APMs