On November 2, 2021, the Centers for Medicare & Medicaid Services (CMS) released the 2022 Physician Fee Schedule (PFS) Final Rule which governs MIPS and other quality payment programs. Anticipated changes were made to MIPS, making the program more challenging in 2022 and signaling additional changes to the program in coming years.
Why You'll Be in For a MIPS Shock - No More Bonus Points or Loopholes
Topics: MACRA & MIPS, Quality Performance Category, IA Performance Category, Cost Performance Category, PI Performance Category, MIPS Value Pathways, 2022 PFS Final Rule
This Could Be Your First Year to Receive a MIPS Penalty. Here's Why.
With the release of the 2020 feedback report detailing the 2.2% maximum possible payment adjustment and the release of the 2022 Final Rule, CMS has demonstrated that MIPS will be both financially rewarding and challenging, in terms of reporting requirements, in 2021 and beyond.
Topics: Quality Performance Category, IA Performance Category, Cost Performance Category, PI Performance Category, 2022 PFS Final Rule
The last 90 days of the year. Many might be ready to say goodbye to 2020 as a year filled with challenges, adjustments and ever-shifting expectations in our personal and professional lives. For those clinicians who are eligible for participation in the Merit-Based Incentive Payment System (MIPS), the last 90 days of the year also represents the beginning of some measurement periods and the final opportunity to improve in others.
Topics: PRO Tips, MACRA & MIPS, Quality Performance Category, IA Performance Category, Cost Performance Category, PI Performance Category
Everything You Need To Know About MIPS Improvement Activities In 2019
The CY 2019 Medicare Physician Fee Schedule Final Rule involves a slew of regulatory changes that will apply to the 2019 performance year. Of course, wading through the final rule to find and understand the most important features of the policy can be grueling; but you’re in luck, because we’ve already done it so you don’t have to! In today’s blog, we’re focusing on the MIPS Improvement Activities (IA) category.
Topics: MACRA & MIPS, Policy, IA Performance Category
With the first performance year of the Merit-based Incentive Payment System (MIPS) drawing to a close, you may have just started getting accustomed to how MIPS reporting works. Although the 2018 MACRA final rule introduced changes to how MIPS performance data should be captured for the upcoming performance year, it may be a relief to hear that largely the changes just build upon the existing 2017 regulations.
Topics: MACRA & MIPS, Policy, Quality Performance Category, ACI Performance Category, IA Performance Category, Cost Performance Category
Statistically, you aren’t sure how you’re supposed to comply with quality reporting requirements this year. As late as June 2017, the majority of providers were still unfamiliar or only somewhat familiar with MACRA; only 9 percent described themselves as “very familiar”. But unless you’re a part of that 9 percent, we highly recommend that you take some time ASAP to familiarize yourself with the requirements and to make a plan for the rest of the year. And as part of that plan, here are four reasons why we recommend that you select Improvement Activities for your practice today (yes, literally today):
Topics: PRO Tips, MACRA & MIPS, IA Performance Category
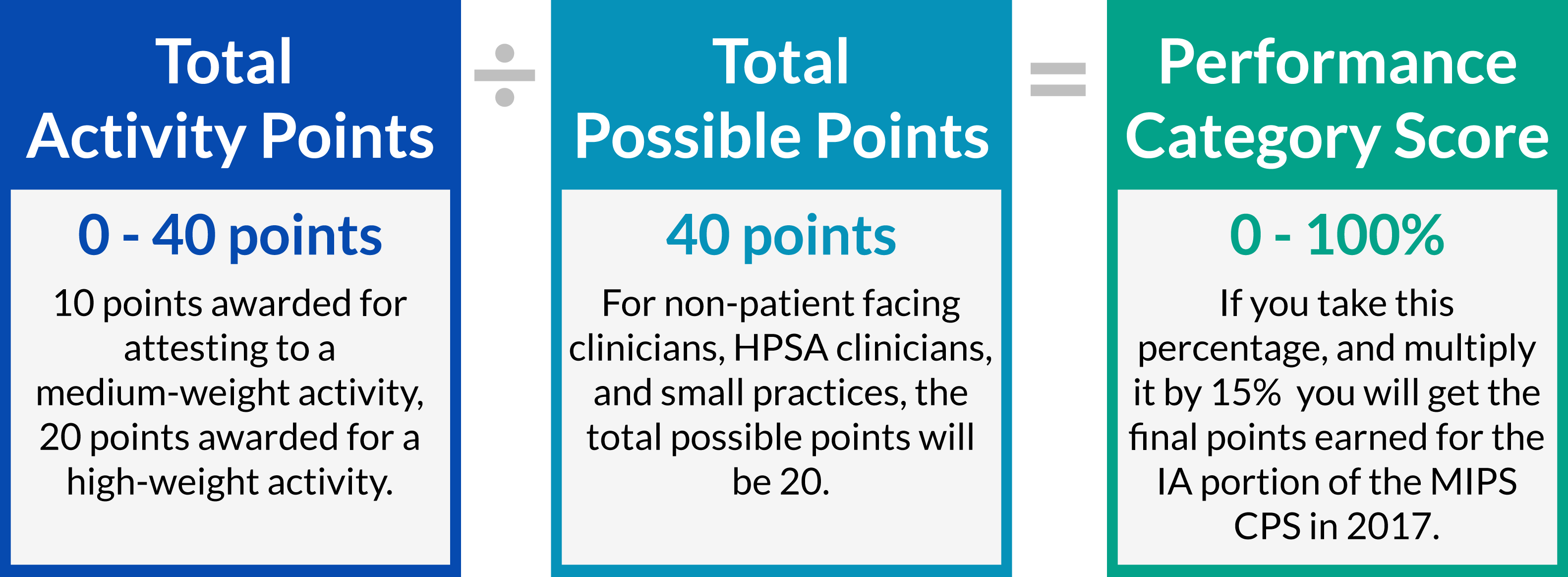
The Improvement Activities Performance Category of MIPS is the the newest quality improvement initiative from CMS. Reporting this category is relatively simple, entailing only that eligible clinicians or groups attest to completing between one and four out of 92 pre-selected improvement activities. Selecting Improvement Activities and understanding how the impact your MIPS final score can be tricky. Luckily, it doesn't have to be!
Topics: PRO Tips, MACRA & MIPS, Policy, IA Performance Category
The Improvement Activities Performance Category is a new concept introduced by MIPS reporting and rewards eligible clinicians for participating in activities related to their patient population. Clinicians and groups can choose to participate in activities most relevant to both their practice and patient population. The Improvement Activities Performance Category is worth 15% of the MIPS Composite Performance Score in 2017.
Topics: MACRA & MIPS, Policy, IA Performance Category
Satisfy the MIPS Improvement Activities Performance Category by Giving Feedback About MACRA!
With the introduction of MIPS reporting in 2017, and the launch of MIPSPRO, now is the time to be considering efficient ways of fulfilling MIPS requirements. CMS is conducting a study with the aim of better understanding practice's experiences quality reporting that will satisfy the Improvement Activities Performance Category of the Merit-Based Incentive Payment System (MIPS). Applications for this study are going to be accepted from January 1 - 31, 2017.
Topics: PRO Tips, MACRA & MIPS, Policy, IA Performance Category
Today, the Department of Health and Human Services (HHS) released the final rule with comment period for the Quality Payment Program under MACRA. Consistent with what was discussed in the proposed rule, the MACRA Quality Payment Program will have two tracks: (1) Advanced Alternative Payment Models (APMs) and the Merit-Based Incentive Payment System (MIPS).
Topics: MACRA & MIPS, Policy, Quality Performance Category, ACI Performance Category, IA Performance Category, Cost Performance Category