In December we posted about a CMS announcement related to ICD-10 diagnosis and procedure code changes, and how this might affect payment adjustments in 2018. At the time CMS had not yet issued their addendum detailing specific code updates for measures being used in the Merit-Based Incentive Payment System (MIPS), but now that they have, here’s an update:
CMS and the National Library of Medicine (NLM) have published the addendum to the 2016 eCQM specifications which affects ICD-10 Clinical Modification (CM) and Procedure Coding System (PCS) value sets for 2017. Health Quality Measure Format (HQMF) specifications, value set object identifiers (OIDs), and measure version numbers for 2017 were not changed. The eCQM value set addendum for 2017 is published to the eCQM Library and the eCQI Resource Center. The NLM’s Value Set Authority Center also provides a complete list of revisions to the eCQM value sets.
Medicare for all?
"We’re going to have insurance for everybody,” President-elect Donald Trump told the Washington Post in an interview over the weekend. "I don’t want single-payer. What I do want is to be able to take care of people.” So while we hear of Affordable Care Act (ACA, sometimes called Obamacare) repeal during the first 100 days of the administration, it sounds as if new programs must be quickly in the works to meet his mandate. “ The Congress can’t get cold feet because the people will not let that happen,” Trump continued, giving further emphasis to his push (and probably tweets) behind this initiative.
Topics: Policy
Satisfy the MIPS Improvement Activities Performance Category by Giving Feedback About MACRA!
With the introduction of MIPS reporting in 2017, and the launch of MIPSPRO, now is the time to be considering efficient ways of fulfilling MIPS requirements. CMS is conducting a study with the aim of better understanding practice's experiences quality reporting that will satisfy the Improvement Activities Performance Category of the Merit-Based Incentive Payment System (MIPS). Applications for this study are going to be accepted from January 1 - 31, 2017.
Topics: PRO Tips, MACRA & MIPS, Policy, IA Performance Category
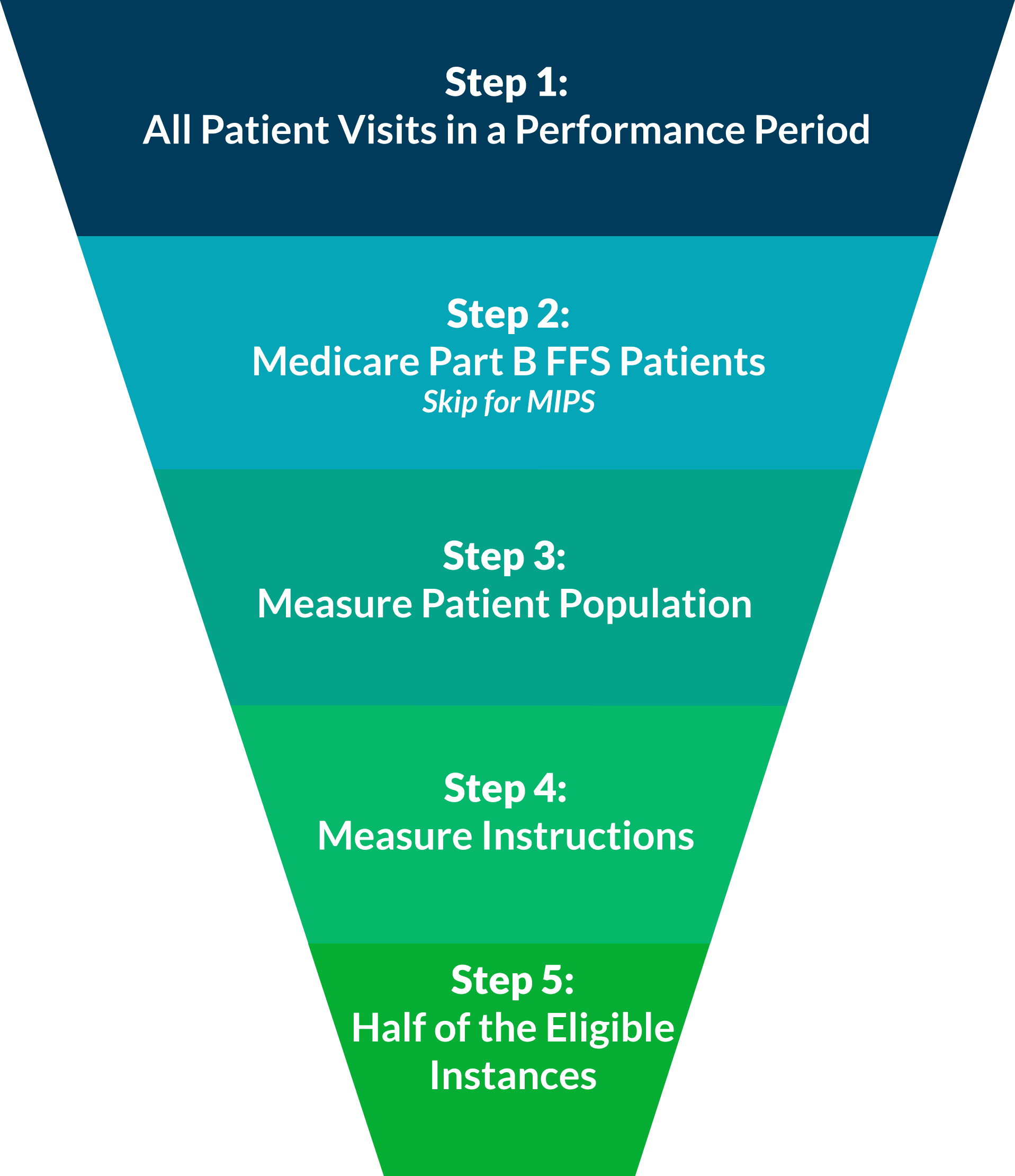
When reporting individual quality measures, whether it be for PQRS this year, or for one of the performance categories of MIPS next year, you are expected to report at least 50% of your eligible instances for each measure. In our experience, this concept can be confusing when practically applied. Luckily, it can be disambigusted in five easy steps!
Consider All Patient Visits for the Performance Period
A performance period for PQRS is based on a complete calendar year beginning on January 1 and ending on December 31.
For MIPS reporting, the performance period can range from a continuous 90-day period to the full calendar year.
Last night, a very surprising article was promoted, "CMS waves Physician Quality Reporting System penalties for 2017, 2018 after massive ICD-10 update clogs system." This post makes it seem as if only the Value-Based Modifier (VM) program penalties and incentives would still be in effect based on PQRS reporting done in 2015 and 2016. This is a dangerous misconception.
Once you've selected how you will report, the next step is to determine what you will report. This is called your reporting method. You have two options: reporting a measures group or reporting individual measures.
Last week, we discussed the first step to reporting PQRS in 2016, selecting a submission mechanism. To briefly recap, there are three submission mechanisms that are viable for practices starting to report at this point in the year: Registry, EHR, and QCDR. Of these three options, Registry reporting has the highest rate of success and ease of submission.
Reporting PQRS in 2016 is just as important as ever, with up to 6% of your Medicare Part B reimbursements on the line in 2018. According to the latest PQRS experience report[1], about 66% of eligible providers are participating in PQRS. Of these participating providers, 68% are still reporting using the claims-based reporting mechanism, which has an abysmal 40% success rate in avoiding the PQRS penalty. Just taking these numbers into account, this takes us up to at least 61% of PQRS eligible providers not avoiding the PQRS penalty.
Top Three Questions about Advanced Alternative Payment Model (APM) Participation
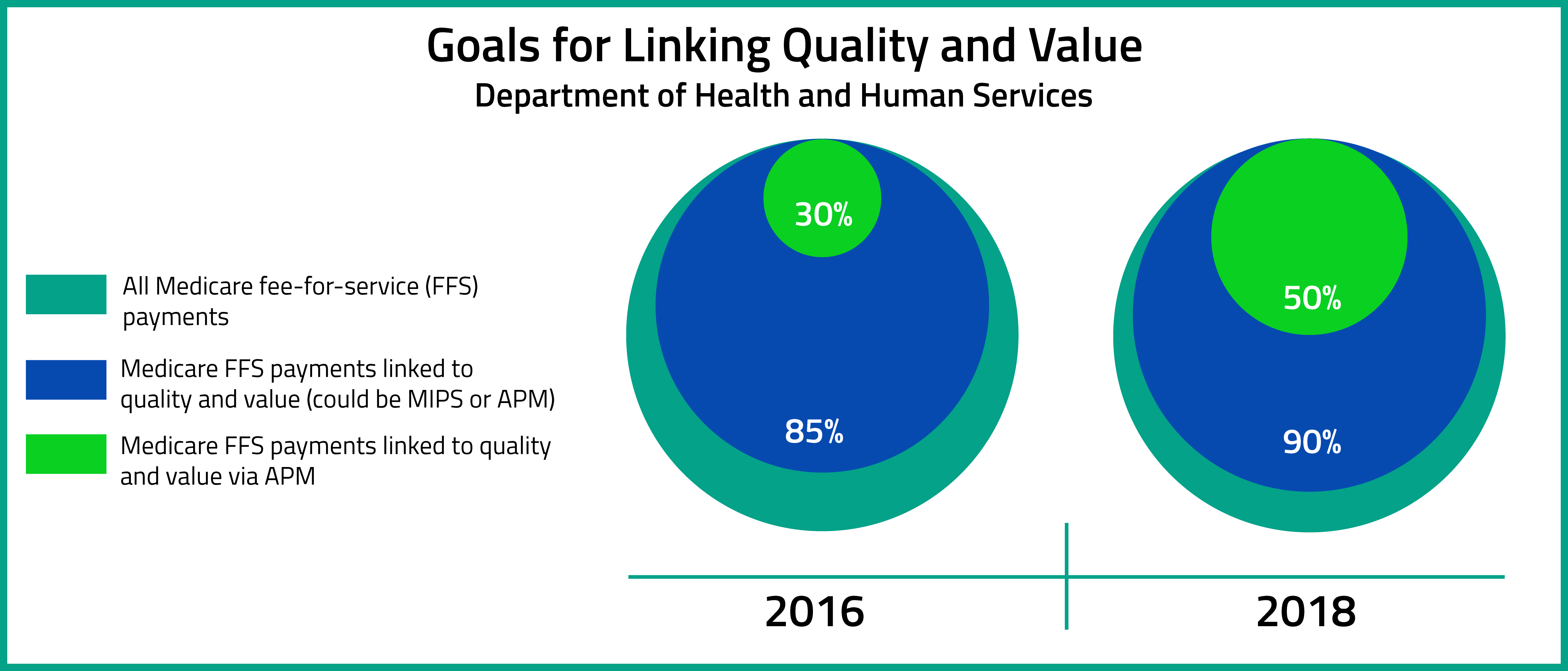
On October 14, 2016, the Department of Health and Human Services release the MACRA Quality Payment Program Final Rule. According to the Executive Summary of the Final Rule, the aims of the Quality Payment Program are to : "(1) support care improvement by focusing on better outcomes for patients, decreased provider burden, and preservation of independent clinical practice; (2) promote adoption of Alternative Payment Models that align incentives across healthcare stakeholders; and (3) advance existing efforts of Delivery System Reform, including ensuring a smooth transition to a new system that promotes high-quality, efficient care through unification of CMS legacy programs."[1]
Topics: MACRA & MIPS, Policy, Eligibility, APMs
Advancing Care Information in the Quality Payment Program Final Rule
The MACRA Quality Payment Program final rule, released Oct. 14, finalizes the payment programs for physicians under MACRA’s Advanced Alternative Payment Models (APMs) and the Merit-Based Incentive Payment System (MIPS), beginning January 1, 2017.
Topics: MACRA & MIPS, Policy, ACI Performance Category
Recently, we highlighted one of the fastest growing types of initiatives for improving the delivery of value-based care--the bundled payment model--and offered some popular opinions about why it is taking off. This week we’ll dive into some specific bundled payment initiatives past and present.
Topics: Bundled Payments, Policy